Understanding the Link Between Testosterone Replacement Therapy and Blood Clot Risk
Introduction
Testosterone replacement therapy, also called TRT, is a medical treatment that has become more common in recent years. It is used when the body does not make enough testosterone on its own. Testosterone is the main male sex hormone, and it plays an important role in energy, mood, muscle growth, bone strength, and sexual health. As men get older, or when certain medical problems affect the body’s ability to produce testosterone, levels of this hormone can drop too low. When this happens, doctors may recommend TRT to bring levels back to normal.
TRT can improve many symptoms linked to low testosterone. Men who take it often report higher energy, improved strength, better sexual function, and a stronger sense of well-being. Because of these benefits, the number of prescriptions for TRT has grown around the world. More men in their 40s, 50s, and 60s are asking about it, and some younger men with specific conditions also receive treatment. But with this increase in use comes new questions about long-term safety.
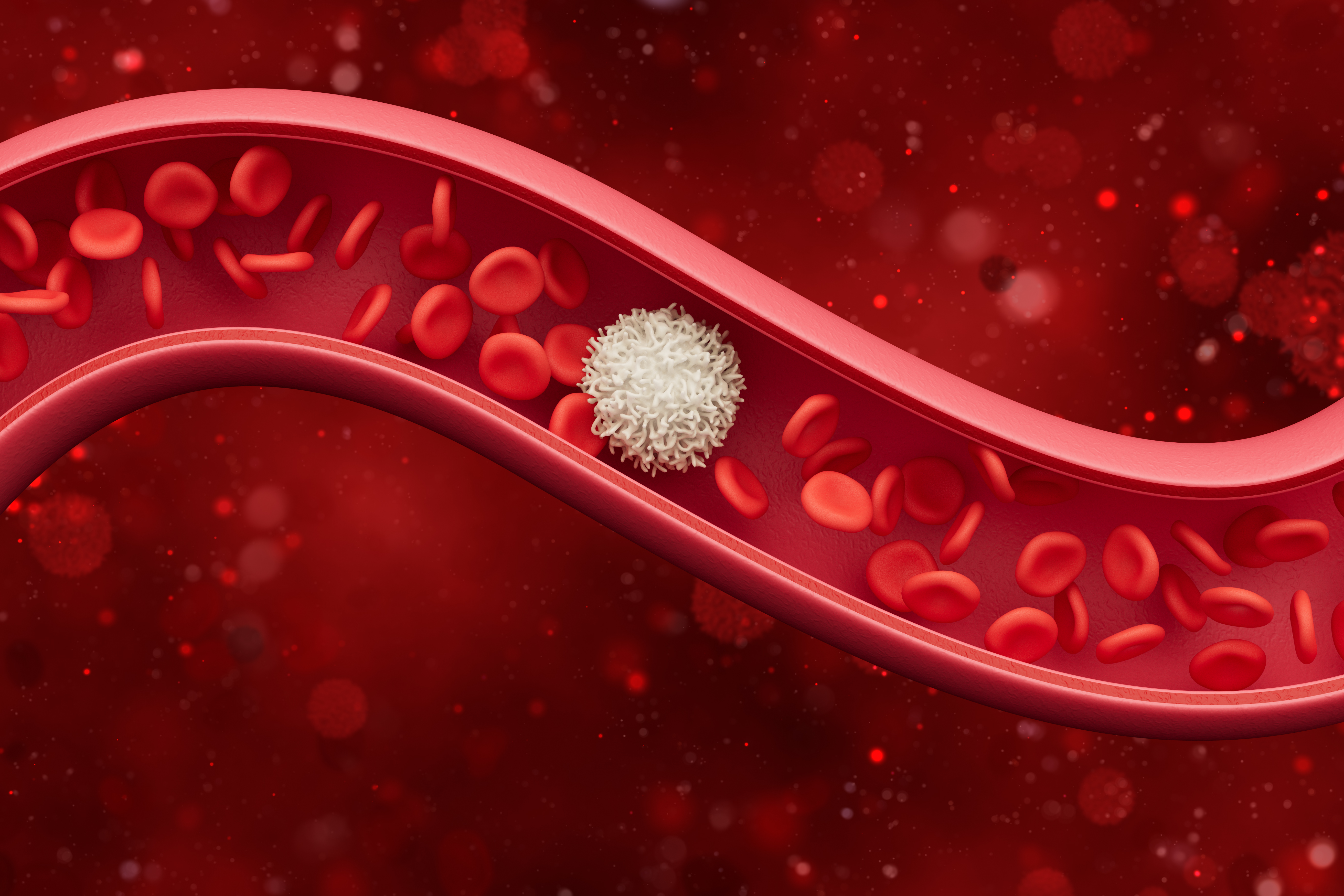
One of the biggest medical questions today is whether TRT raises the risk of developing blood clots. Blood clots are thickened clumps of blood that can block blood flow in veins or arteries. While blood clots are part of the body’s natural healing process, they can become dangerous when they form in the wrong place or at the wrong time. A clot in a deep vein, usually in the leg, is called a deep vein thrombosis (DVT). If part of that clot breaks loose and travels to the lungs, it becomes a pulmonary embolism (PE), which can be life-threatening. Together, DVT and PE are called venous thromboembolism (VTE). Because these conditions can cause serious harm or even death, any possible connection between TRT and clotting needs to be taken seriously.
Researchers have been studying the possible link between TRT and blood clots for more than a decade. Some studies suggest there may be a higher risk, especially in certain groups of patients, while other research shows little or no connection. The U.S. Food and Drug Administration (FDA) has even issued warnings in the past, reminding patients and doctors to be cautious and to weigh risks and benefits carefully. Professional medical groups, such as the Endocrine Society, have also updated their guidelines to address these safety concerns.
For patients, all of this can be confusing. On one hand, TRT may improve quality of life for men who struggle with low testosterone. On the other hand, the idea that it might raise the chance of developing a dangerous blood clot is worrying. Many people turn to the internet with their questions: Does testosterone therapy cause blood clots? Who is most at risk? How can risks be reduced? Are some forms of TRT safer than others? What are the warning signs to watch for?
This article is written to answer the top 10 most common questions about TRT and blood clot risk. It aims to explain the current science in clear, understandable terms. Each section will look at one important part of the issue, from how testosterone affects blood circulation to what patients should ask their doctors before starting therapy. The goal is not to scare people away from TRT, nor to promise it is completely safe. Instead, the purpose is to give readers balanced, factual information so they can have informed conversations with their healthcare providers.
By the end of this article, readers will understand what testosterone therapy is, how it works in the body, what the latest research says about blood clot risk, who may be more vulnerable, and what steps can be taken to lower that risk. They will also know what symptoms to look out for and what to do if they suspect a blood clot. Most importantly, they will see why regular medical supervision is critical when taking TRT.
Blood clot risk is only one piece of the larger picture when it comes to testosterone therapy. But because clots can be so dangerous, it is one of the most important questions to explore in detail. As we move through the next sections, we will look closely at the connection between TRT and clotting, guided by the most frequently asked questions men and their families bring to doctors and search engines alike.
What Is Testosterone Replacement Therapy?
Testosterone replacement therapy, often called TRT, is a medical treatment that helps men who have low levels of testosterone. Testosterone is the main male sex hormone, but it does much more than affect sex drive. It also plays an important role in building muscle, keeping bones strong, making red blood cells, and supporting mood and energy. When testosterone levels drop too low, it can lead to a condition called hypogonadism. TRT is prescribed to bring hormone levels back into a normal range.
Why Doctors Prescribe TRT
There are two main reasons why a doctor might prescribe testosterone therapy:
- Medical Hypogonadism (Primary or Secondary)
- Some men have problems with their testicles or pituitary gland that prevent them from making enough testosterone. This is called medical hypogonadism.
- Causes include genetic disorders, injuries, certain infections, or problems after cancer treatment.
- For these men, TRT can restore testosterone to a healthy level and prevent long-term complications such as weak bones or loss of muscle.
- Age-Related Decline
- Testosterone levels naturally go down as men age, starting around age 30.
- Some men develop bothersome symptoms, such as low energy, reduced strength, depression, or trouble with sexual function.
- In these cases, some doctors may consider TRT, though there is ongoing debate about whether age-related treatment is always needed or safe.
Common Symptoms of Low Testosterone
Before TRT is considered, men usually show signs such as:
- Fatigue or low energy
- Loss of muscle or strength
- Increase in body fat
- Low sex drive or erectile problems
- Trouble concentrating or memory issues
- Mood changes, such as irritability or sadness
Doctors usually confirm low testosterone with a blood test before prescribing TRT.
How TRT Is Given
There are several ways that testosterone can be replaced. Each has its pros and cons.
- Injections
- Testosterone can be injected into the muscle every one to two weeks, or sometimes given as a longer-acting shot that lasts several weeks.
- This method usually raises testosterone levels quickly, but levels may rise and fall between doses, which can cause mood or energy swings.
- Gels and Creams
- These are applied daily to the skin, usually on the shoulders or upper arms.
- They provide a steady amount of testosterone.
- However, there is a small risk that the hormone can transfer to others through skin contact if not careful.
- Patches
- Testosterone patches are worn on the skin and replaced daily.
- They give a steady dose but can sometimes cause skin irritation.
- Pellets
- Small pellets are placed under the skin during a minor procedure in the doctor’s office.
- They release testosterone slowly over three to six months.
- This method avoids daily or weekly dosing but requires a small surgery for insertion.
- Other Forms
- In some countries, testosterone pills, nasal gels, or buccal tablets (placed in the mouth) may also be available.
- Each has specific pros and cons, but all aim to keep testosterone in the healthy range.
How Common Is TRT?
The use of testosterone therapy has grown a lot over the past 20 years. More men are being tested for low testosterone, and more are being prescribed TRT. In the United States alone, millions of prescriptions are written each year.
- This increase is partly due to more awareness of “low T” symptoms.
- However, some experts worry that TRT may sometimes be prescribed without full testing or without clear medical need.
- Because TRT affects many body systems, it is important that men are carefully checked before and during treatment.
TRT is a medical treatment designed to restore testosterone to healthy levels in men with low hormone production. It can improve energy, mood, sexual health, and muscle strength. Doctors prescribe it for men with true hormone deficiencies and sometimes for age-related decline. TRT can be given in several forms, including injections, gels, patches, or pellets. While it is becoming more common, TRT is not without risks, which is why careful medical evaluation and monitoring are essential.
How Does Testosterone Affect the Blood and Circulation?
Testosterone is a hormone that plays a central role in many body systems. Most people know it as the main male sex hormone, but it does much more than affect sex drive, muscle mass, or energy levels. One of the lesser-known roles of testosterone is its effect on the blood and circulation. Understanding this connection helps explain why testosterone replacement therapy (TRT) may be linked to the risk of blood clots in some people.
Testosterone and Red Blood Cell Production
One of the most direct effects of testosterone on the blood is its ability to increase the production of red blood cells. Red blood cells are the carriers of oxygen in the body. They travel through blood vessels, delivering oxygen to tissues and removing carbon dioxide.
Testosterone acts on the bone marrow, which is the “factory” where red blood cells are made. When testosterone levels rise, bone marrow cells are stimulated to produce more red blood cells. This process is called erythropoiesis. While having enough red blood cells is essential for good health, producing too many can create problems.
When red blood cell counts climb too high, the blood can become thicker, a condition known as polycythemia. Thicker blood flows more slowly and is harder for the heart to pump. This increase in thickness, also called blood viscosity, can raise the chance of clots forming inside blood vessels.
Testosterone and Hemoglobin
Along with boosting red blood cells, testosterone also raises levels of hemoglobin, the protein inside those cells that carries oxygen. Higher hemoglobin levels usually mean better oxygen delivery to the body, which can improve stamina and energy. However, if hemoglobin and red blood cell counts become too high, the same risks of thicker blood apply.
Doctors often check hematocrit (the percentage of blood made up of red blood cells) when monitoring patients on TRT. A high hematocrit is a sign that testosterone may be pushing the blood toward a state that increases clot risk.
Testosterone and Platelet Activity
Platelets are another type of blood cell. Their main job is to help blood clot when a person is injured. Normally, this is life-saving because it prevents excessive bleeding. But if platelets become overactive, they can contribute to dangerous clots forming inside veins or arteries.
Some research suggests that testosterone may make platelets more “sticky,” meaning they are more likely to clump together. Sticky platelets can create clots even when there is no injury. This may be one of the ways testosterone therapy adds to clotting risk, though more studies are still needed.
Testosterone, Blood Vessels, and Circulation
Testosterone also affects the lining of blood vessels, known as the endothelium. The endothelium helps regulate blood flow, vessel flexibility, and clotting balance. Healthy testosterone levels may support normal vessel function, but sudden changes in hormone levels from TRT could upset this balance.
Testosterone can also interact with other hormones and chemical messengers that control how wide or narrow blood vessels are. Narrower vessels can increase blood pressure and slow circulation, which in turn may make clotting more likely.
Why This Matters for TRT
For patients using testosterone replacement therapy, these effects highlight why regular monitoring is so important. Doctors will usually check blood counts and watch for early signs of thickened blood. The goal is to balance the benefits of TRT—such as improved energy, mood, and muscle strength—while reducing risks linked to circulation and clotting.
Testosterone is not just a “male hormone.” It is also a powerful regulator of blood and circulation. Understanding how it interacts with red blood cells, platelets, and blood vessels helps explain why researchers are carefully studying the connection between TRT and blood clot risk.
Can Testosterone Therapy Increase the Risk of Blood Clots?
When people think about starting testosterone replacement therapy (TRT), one of the most common questions is whether it raises the chance of developing blood clots. A blood clot is a clump of blood that changes from liquid to a thicker, gel-like state. Clots are not always dangerous. In fact, clotting is the body’s natural way to stop bleeding after an injury. But when clots form inside the veins without an injury, they can block normal blood flow. This can lead to serious problems such as deep vein thrombosis (DVT) or pulmonary embolism (PE).
Evidence From Studies
Doctors and researchers have studied TRT and clotting risk for many years, but the results are not always the same. Some studies show a higher risk, while others do not. This is why the subject is still debated in medicine.
- Large studies: Some large medical studies have found that men who start TRT may have a slightly higher chance of developing clots in the first six months of therapy. After that period, the risk seems to go back to normal.
- Other studies: On the other hand, some research shows no major link between TRT and clots, especially in men who are healthy and carefully monitored.
- FDA warning: Because of the mixed results, the U.S. Food and Drug Administration (FDA) requires TRT products to carry a warning about possible clot risks. This is meant to alert patients and doctors to be cautious.
In summary, the scientific evidence is mixed, but there is enough concern for health agencies to ask for caution.
How TRT Might Increase Clot Risk
Even though not every study shows the same result, doctors understand several ways that testosterone might make clots more likely.
- Thicker blood (polycythemia): Testosterone encourages the body to make more red blood cells. While this can help men with low levels feel more energetic, too many red blood cells can make the blood thicker. Thick blood flows more slowly and can raise the chance of clot formation.
- Changes in clotting proteins: Some studies suggest that testosterone may influence proteins in the blood that help it clot. This could make the blood more likely to form clots in certain people.
- Platelet activity: Platelets are small cells that help blood clot. There is some evidence that testosterone might make platelets more “sticky,” which could increase clot risk.
- Indirect effects: TRT can also cause changes in weight, cholesterol levels, and blood pressure. These changes may indirectly influence clot risk, especially in men who already have other health problems.
Types of Blood Clots Linked to TRT
Not all clots are the same. The two most serious types linked to testosterone therapy are:
- Deep Vein Thrombosis (DVT): This is when a clot forms in a deep vein, often in the legs. Symptoms include pain, swelling, and redness. If not treated, a piece of the clot can break off and travel to the lungs.
- Pulmonary Embolism (PE): This happens when a clot travels to the lungs and blocks blood flow. Symptoms include sudden shortness of breath, chest pain, rapid heartbeat, or feeling lightheaded. PE can be life-threatening and requires emergency care.
Why the Risk May Be Higher Early On
Many studies show that if TRT does raise clot risk, it is most noticeable in the first few months after starting therapy. This may be because the blood adjusts quickly to the sudden increase in testosterone. During this adjustment period, red blood cell counts can rise quickly, making blood thicker than normal. Over time, the body may adapt, and the risk seems to decrease.
Differences Between Individuals
It is important to note that not everyone on testosterone therapy will face the same risk. Factors that can make clotting more likely include:
- Being older.
- Having a history of clots.
- Being overweight.
- Smoking.
- Having certain inherited conditions that affect blood clotting.
For these groups, the effect of TRT on clot risk may be stronger.
The link between testosterone therapy and blood clots is not completely settled. Some men may face little to no extra risk, while others may be more vulnerable. What is clear is that testosterone can make blood thicker and affect clotting in ways that deserve attention. Because of this, men on TRT should be carefully monitored with regular blood tests and follow-ups. Doctors often check hemoglobin and hematocrit levels, which show how concentrated red blood cells are. If levels get too high, treatment may need to be adjusted or paused to reduce clot risk.
Who Is Most at Risk for Clotting While on TRT?
Not everyone who takes testosterone replacement therapy (TRT) has the same risk of developing a blood clot. Some people are more likely to experience clotting problems than others. This difference depends on age, health history, lifestyle, and certain inherited conditions. Understanding these risks is important before starting therapy and while continuing treatment.
Age-Related Risks
Age plays a big role in blood clot risk.
- Older adults: As people age, the natural ability of the blood vessels and the heart to function smoothly can weaken. Blood flow may slow down, and veins can become less elastic. This can raise the chance of clot formation. Older men who use TRT may have a higher risk compared to younger men.
- Middle-aged adults: Men in their 40s and 50s are often the largest group receiving TRT. At this age, health problems like high blood pressure, high cholesterol, or diabetes may also appear, which can add to clot risk.
- Younger men: While rare, younger men can still develop clots if they already have genetic clotting conditions or other health factors.
Pre-Existing Medical Conditions
Several medical conditions increase the risk of clots, and these risks can become stronger when combined with TRT.
- Obesity: Extra weight can place pressure on the veins, especially in the legs. This slows down blood return to the heart and raises the risk of deep vein thrombosis (DVT). TRT may add to this risk by making the blood thicker.
- Cardiovascular disease: Heart disease, high blood pressure, and high cholesterol all strain the circulatory system. When TRT raises red blood cell counts, the thicker blood can put extra pressure on blood vessels already damaged by these conditions.
- Diabetes: This condition affects blood vessels and circulation. Combined with TRT, diabetes may raise the chance of clotting problems.
- Previous clotting history: A man who has had a DVT, pulmonary embolism, or any other clotting problem before is more likely to have another clot if starting TRT.
Genetic or Inherited Clotting Disorders
Some people are born with conditions that make the blood more likely to clot. These inherited disorders may not always cause problems until later in life or until combined with other risks, such as TRT. Examples include:
- Factor V Leiden mutation: A common genetic change that increases clotting tendency.
- Prothrombin gene mutation: Another inherited condition linked to blood clot risk.
- Protein C or Protein S deficiency: Rare conditions where the natural proteins that prevent clots do not work properly.
For men with these conditions, TRT may act like an extra trigger, pushing the blood toward clot formation. Doctors often recommend genetic testing if there is a strong family history of blood clots before prescribing TRT.
Lifestyle Factors
How a person lives day to day can also change clotting risk.
- Smoking: Cigarette smoke damages blood vessels, making clots more likely. When combined with TRT, this can create a stronger risk.
- Sedentary lifestyle: Sitting for long hours, such as at a desk job or during long travel, slows blood circulation in the legs. If TRT makes the blood thicker, the chances of a clot in the legs go up.
- Poor hydration: Not drinking enough fluids can make blood more concentrated and sluggish. This makes it easier for clots to form.
- Alcohol use: Heavy drinking can harm the liver, which helps control clotting factors. This can upset the balance between bleeding and clotting.
Medication Interactions
Some medicines can also affect clot risk. For example:
- Estrogen-containing drugs: If a man is also taking estrogen therapy (rare, but possible in certain conditions), the combined effect with TRT may increase clotting.
- Corticosteroids: Long-term use can raise blood pressure and affect clotting.
- Certain cancer treatments: Some treatments make blood more likely to clot, and TRT may add to this problem.
Men at the highest risk for clots while on TRT often have more than one of these factors. For example, an older man who is overweight, has high blood pressure, and smokes will be at far greater risk than a healthy younger man with no medical history.
Doctors usually look at the whole picture before prescribing TRT. They may recommend more frequent blood tests for men with several risk factors, or they may decide that TRT is not safe at all.
TRT does not affect everyone in the same way. The risk of blood clots is highest in men who already have health problems, genetic clotting issues, or lifestyle habits that make clots more likely. Knowing your personal risk helps you and your doctor make safer decisions about starting or continuing testosterone therapy.
What Are the Signs and Symptoms of a Blood Clot?
When someone is taking testosterone replacement therapy (TRT), one concern is the possible risk of developing a blood clot. A blood clot forms when blood thickens and clumps together inside a vein or artery. While clots can sometimes help stop bleeding after an injury, they can also be dangerous if they form where they should not. A clot that blocks normal blood flow can cause swelling, pain, or even life-threatening problems if it travels to the lungs.
This section explains the main signs and symptoms of blood clots, focusing on two common types: deep vein thrombosis (DVT) and pulmonary embolism (PE). Knowing these warning signs is important so that people can get medical help right away.
Deep Vein Thrombosis (DVT)
What it is:
Deep vein thrombosis happens when a clot forms in a deep vein, usually in the legs. The clot blocks blood from moving back to the heart as it should, which leads to swelling and discomfort.
Common symptoms of DVT include:
- Swelling in the leg or arm
- Usually happens on one side of the body, not both.
- The swelling may come on suddenly or slowly over several days.
- Shoes, socks, or pants may feel tighter than normal.
- Pain or tenderness
- The pain often feels like a cramp or soreness in the calf or thigh.
- It may get worse when standing or walking.
- Sometimes the pain is mild and can be mistaken for muscle strain.
- Skin changes
- The skin over the clot may look red or discolored.
- The area may feel warm to the touch.
- In some cases, the skin looks pale or bluish if blood flow is blocked.
- Heaviness or tired feeling
- The affected leg may feel heavier than usual.
- Some people describe it as dragging their leg when walking.
DVT can sometimes go unnoticed, especially if the clot is small. But even a small clot can grow larger or break loose, leading to serious problems.
Pulmonary Embolism (PE)
What it is:
A pulmonary embolism happens when a clot breaks free and travels through the bloodstream to the lungs. This is a medical emergency because the clot blocks blood from reaching lung tissue, which reduces oxygen levels in the body.
Common symptoms of PE include:
- Shortness of breath
- May come on suddenly, even at rest.
- Can feel like not being able to catch a full breath.
- Often worsens with physical activity.
- Chest pain
- Sharp or stabbing pain that may feel worse with deep breathing or coughing.
- Sometimes mistaken for a heart attack.
- Cough
- May be dry or produce bloody or blood-streaked mucus.
- Rapid heartbeat
- The heart races to move blood around the blocked area.
- Some people also feel lightheaded or faint.
- Feeling anxious or dizzy
- Sudden dizziness, sweating, or a sense of panic can signal a serious blockage.
Pulmonary embolism can be fatal if not treated quickly. That is why anyone with sudden chest pain or shortness of breath should call emergency services right away.
When to Seek Medical Attention
Blood clots are dangerous because they may grow or travel to vital organs. Immediate medical attention is needed if you notice any of the following:
- Swelling and pain in one leg that does not improve.
- Sudden, unexplained shortness of breath.
- Sharp chest pain that gets worse when breathing deeply.
- Coughing up blood.
- Dizziness, fainting, or rapid heartbeat.
Doctors use tests such as ultrasound, CT scans, and blood work to confirm whether a clot is present. If found early, blood clots can often be treated with medications that thin the blood and prevent the clot from getting bigger.
Why Recognizing Symptoms Matters for TRT Users
People using testosterone therapy should be extra alert to the signs of blood clots. TRT may increase red blood cell count, which thickens the blood and raises the chance of clotting. While not everyone on TRT will face this risk, recognizing symptoms early gives the best chance for safe treatment.
How Do Doctors Evaluate Clot Risk Before Starting TRT?
Before starting testosterone replacement therapy (TRT), doctors must make sure it is safe for each patient. Testosterone affects the blood, the heart, and circulation. Because of this, one of the most important steps is checking the risk of blood clots. A blood clot is when blood thickens and sticks together inside a vein or artery. This can block normal flow and cause serious health problems, such as deep vein thrombosis (DVT) in the legs or a pulmonary embolism (PE) in the lungs.
Evaluating clot risk means looking at a patient’s medical history, performing tests, and asking the right questions. Below, we will go through the main steps doctors use to decide if TRT is safe.
Reviewing Medical and Family History
The first step is a detailed health history. Doctors ask about:
- Past blood clots: If a patient has had DVT, PE, or another clot before, the chance of having another one is higher. TRT may make that risk greater.
- Family history: Some people inherit blood clotting problems. If close relatives have had clotting disorders or strokes at a young age, this could be a warning sign.
- Other health conditions: Diseases such as obesity, diabetes, high blood pressure, and cancer can raise clot risk. Conditions that limit movement, such as recent surgery or long hospital stays, can also add risk.
- Lifestyle factors: Smoking, heavy drinking, and little physical activity can contribute to clot formation.
By combining all this information, a doctor can see if a patient belongs to a higher-risk group.
Checking Current Symptoms
Sometimes, people may already have a clot without knowing it. Before prescribing TRT, a doctor may ask about leg pain, swelling, shortness of breath, or chest pain. These can be signs of a clot. If there are concerns, the doctor may order imaging tests, such as an ultrasound of the legs or a CT scan of the chest, before moving forward.
Blood Tests
Doctors also use blood work to help measure risk:
- Hematocrit and hemoglobin: Testosterone increases red blood cell production. If levels are already high, the blood may become too thick (a condition called polycythemia). Thick blood flows more slowly and clots more easily.
- Platelet count: Platelets help blood clot. A high number can increase the chance of unwanted clots.
- Clotting factors: Some tests check how quickly blood clots. For people with a personal or family history of clotting disorders, doctors may order special tests to look for genetic conditions, such as Factor V Leiden mutation or prothrombin gene mutation.
These lab results give an early warning if TRT could push the body toward dangerous clotting.
Screening for Thrombophilia
Thrombophilia means an increased tendency to develop blood clots. Some types are inherited, while others come from medical conditions or medications. People with thrombophilia may need to avoid TRT or be monitored more closely. Tests for thrombophilia look at protein levels (like protein C, protein S, and antithrombin) and genetic markers.
Not every patient will need this kind of testing. Doctors usually order it only if there is a strong personal or family history of clots.
Risk Scoring Systems
Doctors sometimes use scoring tools to measure overall clot risk. These tools consider age, weight, smoking, recent surgery, travel, and history of clotting events. By putting these factors together, a doctor can estimate how likely a clot is in the future. This helps guide the decision about whether TRT is safe or whether extra steps are needed.
When Doctors Delay or Avoid TRT
If the risk is too high, a doctor may decide not to start TRT right away. Instead, they may treat other health problems first. For example:
- If hematocrit is too high, blood may be drawn (a procedure called phlebotomy) to thin it.
- If a patient smokes, quitting will lower clot risk.
- If someone recently had surgery, the doctor may wait until the risk of post-surgical clots is lower.
In some cases, TRT may not be recommended at all, especially if blood clot risk is very high or if the patient is on strong anticoagulant (blood-thinning) medication.
Shared Decision-Making
Finally, the doctor and patient must talk through the risks and benefits together. TRT can improve energy, mood, and sexual health. But it also comes with possible dangers. Understanding the risk of clots helps the patient make an informed choice. Doctors may suggest close follow-up, repeat blood tests every few months, and regular check-ups to adjust the treatment safely.
Before starting TRT, doctors carefully check clot risk. They do this by reviewing medical and family history, looking for symptoms, ordering blood tests, screening for clotting disorders, and sometimes using scoring systems. If risks are found, treatment may be delayed, adjusted, or avoided. This careful evaluation is important to protect patients from serious complications while still giving them the benefits of hormone therapy.
Are All Forms of TRT Equally Risky?
Testosterone replacement therapy (TRT) can be given in several ways. Doctors choose a method based on the patient’s age, health, lifestyle, and preference. While all forms of TRT raise testosterone levels in the body, they do not always act the same. Some cause faster changes, while others release testosterone more slowly. These differences may affect how much the blood thickens, how the heart and vessels respond, and whether there is a higher chance of forming blood clots.
In this section, we will look at the main types of TRT—injections, gels, patches, and implants (pellets)—and discuss how each one might affect blood clot risk.
Injections
Injections are one of the most common forms of TRT. They are usually given into the muscle every 1 to 2 weeks (short-acting) or every 10 to 12 weeks (long-acting).
- Hormone levels: After a shot, testosterone levels in the blood rise quickly and then drop before the next dose. This creates peaks and valleys.
- Impact on blood: The sudden increase can strongly stimulate red blood cell production. This may raise hematocrit (the portion of blood made up of red blood cells). When hematocrit is too high, blood becomes thicker, which can slow flow and increase clot risk.
- Clot concerns: Studies have suggested that men using injections, especially short-acting ones, may have a higher chance of blood thickening compared to other methods. This does not mean every man will get clots, but doctors usually monitor blood counts more closely in patients who receive injections.
Gels
Gels are applied daily to the skin, often on the shoulders or upper arms. The testosterone is absorbed slowly into the blood through the skin.
- Hormone levels: Gels give a steady amount of testosterone each day, so the blood levels stay more even compared to injections.
- Impact on blood: Because the hormone enters gradually, the rise in red blood cells is often slower and less extreme. This may lower the chance of blood becoming too thick.
- Clot concerns: Some studies show that men on gels tend to have fewer problems with high hematocrit compared to injection users. However, they still need monitoring because every body reacts differently.
- Other factors: Gels can be expensive and must be applied daily. There is also a small risk of transferring testosterone to others through skin contact, but this does not directly affect clot risk.
Patches
Patches are placed on the skin, usually once a day, and release testosterone in a controlled way.
- Hormone levels: Like gels, patches provide more stable levels than injections.
- Impact on blood: The effect on red blood cell counts is usually mild. This can make them safer for patients who already have a higher risk of clotting.
- Clot concerns: Evidence suggests patches are among the least likely to cause thickening of the blood. Still, they can cause skin irritation, which may make some people stop using them.
Implants (Pellets)
Pellets are small solid pieces of testosterone placed under the skin, usually in the hip or buttock area. A doctor inserts them during a minor procedure, and they release hormone slowly for 3 to 6 months.
- Hormone levels: Pellets give a steady release, but sometimes the amount can vary if a pellet shifts or dissolves unevenly.
- Impact on blood: Like injections, pellets can stimulate a noticeable rise in red blood cells, especially in the first few months after insertion.
- Clot concerns: Some reports suggest pellets may raise hematocrit more than gels or patches but less than frequent injections. Regular blood testing is needed to watch for changes.
Comparing Risks
When we compare these forms:
- Injections seem to have the strongest effect on red blood cell growth and therefore may carry the highest risk of blood becoming too thick.
- Pellets can also increase blood counts, though usually not as sharply as injections.
- Gels and patches appear to cause fewer problems with blood thickness and may be safer for men at higher risk of clots.
It is important to remember that studies are still ongoing. Not every man will respond the same way. Some may tolerate injections without issues, while others may develop high hematocrit even on gels.
Doctor’s Role in Reducing Risk
No matter which form of TRT is chosen, doctors usually:
- Check blood counts (hematocrit and hemoglobin) every few months.
- Adjust the dose or switch methods if the blood becomes too thick.
- Advise lifestyle changes such as exercise, drinking enough water, and avoiding smoking, which can add to clot risk.
All forms of testosterone therapy can raise blood counts to some degree, which can affect clotting risk. Injections may cause the largest changes, while gels and patches are often gentler. Pellets fall somewhere in between. The safest choice depends on the patient’s health history, preferences, and how their body reacts. Careful monitoring by a doctor is essential, no matter which form is used.
How Can Blood Clot Risk Be Reduced While on TRT?
Testosterone replacement therapy (TRT) can be very helpful for men with low testosterone, but one concern is the possible risk of blood clots. A blood clot can block blood flow and cause serious problems like deep vein thrombosis (DVT) or pulmonary embolism (PE). Because of this, it is very important for patients and doctors to work together to reduce clot risk as much as possible. Below are several ways this can be done.
Regular Monitoring of Blood Counts
One of the main ways testosterone affects the body is by increasing red blood cell production. While this can give more energy and improve well-being, too many red blood cells make the blood thicker. Thick blood moves more slowly and is more likely to form clots.
Doctors check this by measuring hematocrit (the percentage of blood made up of red blood cells) and hemoglobin (the protein that carries oxygen). If these levels go too high, the risk of clotting increases.
- Safe range: Most doctors want hematocrit to stay below 54%.
- How often: Blood tests are usually done before starting TRT, then every 3–6 months during the first year, and at least once a year after that.
- What happens if it’s too high: If hematocrit rises above safe levels, the doctor may lower the TRT dose, change the method of treatment, or pause therapy until the blood returns to normal. Sometimes a process called therapeutic phlebotomy (removing some blood, similar to donating blood) is used to quickly lower hematocrit.
Lifestyle Changes That Lower Risk
Everyday choices can make a big difference in clot risk. Even though TRT might raise red blood cell levels, healthy habits can help keep the blood flowing smoothly.
- Stay active: Moving the body helps keep blood moving. Sitting for long hours, especially on flights or at a desk, raises clot risk. Simple steps like standing up every hour, walking, or stretching can help. Regular exercise, such as walking, swimming, or cycling, improves circulation and lowers overall risk.
- Maintain a healthy weight: Being overweight or obese increases clot risk on its own. Combining obesity with TRT can raise the danger further. A balanced diet and regular exercise can help lower this risk.
- Avoid smoking: Smoking damages blood vessels and increases the chance of clotting. Quitting smoking is one of the best ways to improve overall health and reduce clot risk.
- Stay hydrated: Dehydration makes blood thicker and stickier. Drinking enough water each day can keep blood at the right thickness.
Adjusting TRT Method and Dose
Not all TRT methods affect the blood in the same way. Injections often create higher peaks of testosterone, which may increase red blood cell production more than gels or patches. For men who develop high hematocrit on injections, switching to a skin gel, patch, or implant might lower the risk.
- Lowering the dose may also help. Sometimes doctors adjust the amount of testosterone given to balance benefits with safety.
- Spreading out doses can avoid big spikes in testosterone levels, reducing strain on the body.
Use of Medications in High-Risk Patients
For patients who already have a history of blood clots or strong genetic risk factors, doctors may consider medicines to reduce clotting risk. These medicines include anticoagulants (blood thinners). However, they are not used for everyone, since they carry their own risks, such as bleeding.
The choice depends on the patient’s overall health, personal history, and how necessary TRT is. Only a doctor can decide if blood-thinning medication is appropriate.
Ongoing Medical Supervision
TRT should never be started and then forgotten. Ongoing medical care is essential. Patients should keep all scheduled follow-up visits and report any new symptoms right away. Warning signs like swelling in the legs, chest pain, or sudden shortness of breath should be treated as emergencies.
Good supervision also means checking other health factors. Doctors may watch cholesterol, blood pressure, and heart health, since these also play a role in clot risk.
What Does the FDA and Medical Guidelines Say About TRT and Clot Risks?
When people hear that a medicine might raise the risk of blood clots, they often look to trusted organizations like the U.S. Food and Drug Administration (FDA) and leading medical societies for guidance. Testosterone replacement therapy (TRT) has been under careful review by these groups, especially as more men are using it for low testosterone. This section explains what the FDA has said about TRT and blood clots, what professional medical guidelines recommend, and where the science is still unclear.
The FDA’s Safety Warnings
The FDA is responsible for making sure medicines in the United States are safe and effective. In 2014, the FDA issued a warning about the risk of venous thromboembolism (VTE) with TRT. VTE is a medical term that includes deep vein thrombosis (DVT) and pulmonary embolism (PE).
The FDA noted that there were reports of men developing dangerous clots soon after starting testosterone treatment. These clots happened even in men who did not have a history of clotting disorders. Because of this, the FDA required drug makers to add warnings to testosterone product labels.
By 2015, the FDA also updated its guidance, saying TRT should be used only in men with clear medical causes of low testosterone—such as certain genetic conditions, injury to the testicles, or diseases affecting hormone glands. The FDA advised against routine prescribing of TRT simply for “low testosterone due to aging.” The reason was not only clot risk, but also concerns about heart attack and stroke risk.
In summary, the FDA’s stance is cautious. It allows TRT when medically needed but reminds both doctors and patients that risks like blood clots are real and must be monitored.
Guidance from Professional Medical Societies
Medical groups have also looked at the evidence and created guidelines to help doctors use TRT safely. Here are the main positions:
- Endocrine Society: This group recommends TRT only for men with confirmed low testosterone on repeated blood tests and with symptoms of deficiency. Before starting therapy, doctors should check for conditions that increase clot risk, such as high red blood cell counts, sleep apnea, or a history of DVT or PE.
- American Urological Association (AUA): The AUA also stresses careful testing before TRT. It advises regular monitoring of hematocrit (a measure of red blood cell concentration). If hematocrit goes above a safe range, TRT should be paused or adjusted, because thicker blood can increase clot risk.
- European Association of Urology (EAU): This group supports similar steps. It also notes that men with uncontrolled heart disease or recent clots should avoid TRT until the risks are addressed.
These guidelines show a shared concern: TRT should not be used casually, and anyone on TRT must be monitored closely for changes in blood health.
What the Guidelines Do Not Yet Answer
Even though the FDA and professional societies provide direction, there are still unanswered questions. Large clinical trials that follow men for many years are limited. Some studies show a link between TRT and clots, while others do not. Researchers are still trying to understand:
- Why some men develop clots soon after starting TRT, while others never do.
- Whether certain forms of TRT (injections, gels, or pellets) carry more risk.
- How age, obesity, smoking, or genetic clotting factors interact with TRT.
Because of these unknowns, guidelines tend to be conservative. They lean toward careful patient selection, ongoing monitoring, and cautious dosing until more science is available.
What Patients Should Take Away
For patients, the key message is this: The FDA and major medical groups recognize that TRT can help men with real medical conditions, but it is not risk-free. Blood clots are a serious but uncommon complication. To lower risk, men should:
- Use TRT only when there is a clear medical need confirmed by testing.
- Have their blood checked regularly for red blood cell levels.
- Report symptoms like leg swelling, sudden chest pain, or shortness of breath right away.
- Discuss personal risk factors with their doctor before starting TRT.
The FDA’s warnings and the guidelines from professional groups are designed to protect patients. They do not ban TRT, but they remind us that this treatment is powerful and must be managed carefully. Until more long-term studies are done, TRT should be used thoughtfully, with risks like blood clots kept in focus.
What Should Patients Discuss With Their Doctor?
Starting testosterone replacement therapy (TRT) is not a small decision. It can bring important benefits for men who have low testosterone, such as better energy, stronger muscles, improved mood, and sexual health. But like any medical treatment, TRT also carries risks. One of the main risks that doctors and patients watch closely is the chance of developing blood clots. Because of this, open and detailed conversations between patients and doctors are very important before and during TRT.
Below are key topics that every patient should talk about with their doctor.
Questions to Ask Before Starting TRT
Before beginning treatment, patients should take time to ask about:
- Personal Risk of Blood Clots: Each person’s body and medical history are different. Some men may already have a higher chance of developing a clot because of age, weight, smoking, or family history. Patients should ask: “Based on my health, do I have a higher risk for blood clots?”
- Other Health Problems: Men with heart disease, high blood pressure, diabetes, or previous clotting problems may face more risks. Patients should ask: “Do my other health conditions make TRT unsafe for me?”
- Treatment Goals: Some men may expect major changes quickly. It is helpful to ask: “What results should I realistically expect from TRT, and how long will it take?” Clear goals help doctors and patients track progress safely.
Monitoring and Testing During TRT
TRT requires regular check-ups to stay safe. Patients should know exactly how often they need to return to the clinic for tests and exams. Key monitoring questions include:
- Blood Tests: Testosterone therapy can increase the number of red blood cells in the body. Too many red blood cells can thicken the blood, making clots more likely. Patients should ask: “How often will you check my blood count, and what happens if it gets too high?”
- Clotting Risks: Some doctors may order special clotting tests if a patient has a family history of clot problems. Patients should ask: “Will I need extra tests to check my blood clot risk?”
- Follow-Up Visits: Patients should ask: “How often will I need to come back for follow-up appointments, and what will you check each time?”
Knowing the plan ahead of time can make patients feel more confident and supported.
Possible Warning Signs to Watch For
It is important for patients to learn the early signs of a blood clot so they can get help quickly. During appointments, patients should ask their doctor to explain symptoms in detail. Helpful questions include:
- “What are the signs of a blood clot in the leg that I should never ignore?”
- “What are the signs of a blood clot in the lungs that mean I should call 911?”
Doctors can explain that leg swelling, redness, pain, or warmth may point to a clot in the leg (deep vein thrombosis). Sudden chest pain, trouble breathing, or coughing up blood may signal a clot in the lungs (pulmonary embolism).
Patients should also ask: “If I notice these symptoms, what should I do first?” Knowing the right steps can save lives.
Medication, Lifestyle, and Safety Choices
Beyond regular tests, patients should also talk with their doctor about lifestyle habits and medicine use. Questions include:
- Exercise and Activity: “What kind of exercise is safe for me while on TRT, and how often should I do it?” Regular movement lowers the chance of clots.
- Other Medications: Some drugs, like blood thinners or steroids, may interact with TRT. Patients should ask: “Will TRT affect the other medicines I take?”
- Healthy Habits: Smoking, dehydration, and long periods of sitting raise the risk of clots. Patients should ask: “What daily habits can I change to keep my blood clot risk lower?”
Doctors may recommend staying hydrated, walking daily, and avoiding smoking.
Personalized Risk–Benefit Assessment
Every man’s situation is different. Some patients may have a strong medical need for TRT, while for others the benefits may not outweigh the risks. Because of this, a personal risk–benefit conversation is critical. Patients should ask:
- “Based on my test results and history, do you think the benefits of TRT are worth the risks for me?”
- “If my risks increase while I am on TRT, what other treatment choices will I have?”
This helps patients make informed decisions with their doctor rather than feeling uncertain or rushed.
Before starting or continuing TRT, patients should feel comfortable asking detailed questions about their health, their risks, and their care plan. No question is too small. Open communication with the doctor is the best way to stay safe, prevent serious complications like blood clots, and get the most benefit from treatment.
Conclusion
Testosterone replacement therapy, often called TRT, is a treatment that can help men who have low testosterone levels. It can improve energy, mood, muscle strength, and even sexual health. But while TRT has real benefits, there are also concerns about safety, especially the risk of blood clots. Understanding this link is very important for both patients and doctors.
The science shows that testosterone affects how the blood is made and how it flows through the body. One of its main effects is to increase the production of red blood cells. This is helpful if a person has anemia or low blood counts, but if red blood cells rise too high, the blood becomes thicker. Thick blood flows more slowly and may form clots more easily. These clots can block veins or arteries, which may lead to deep vein thrombosis in the legs or pulmonary embolism in the lungs. Both conditions can be dangerous and require urgent medical care.
Not everyone who uses TRT will develop a blood clot. Many men take testosterone for years without any major problems. But research shows that certain groups are at higher risk. Men who are older, overweight, or who already have heart disease face more danger. People with a history of clotting disorders, such as factor V Leiden mutation, are also more likely to have trouble. Lifestyle choices, like smoking or sitting for long periods, make the risk higher too. This is why doctors do careful screening before starting TRT. They check medical history, order blood tests, and sometimes look for hidden clotting problems.
Different methods of TRT may affect risk in different ways. Injections can cause sudden spikes in testosterone, which may raise blood counts more quickly. Gels and patches often provide steadier hormone levels, which may lower some risks. However, no method is completely free of danger, and research is still ongoing. Because of this, medical guidelines stress that doctors should watch patients closely, no matter which form of TRT they use.
Patients should also know the signs of a blood clot. These include swelling, pain, and redness in the leg, or sudden chest pain and shortness of breath. Knowing these signs can save lives, because early treatment is much more effective than waiting. Anyone on TRT who notices these symptoms should seek medical help right away.
Reducing risk while on TRT is possible. Doctors usually monitor hematocrit and hemoglobin levels, which measure how thick the blood has become. If these numbers go too high, TRT may be paused or adjusted. Sometimes blood donation, called therapeutic phlebotomy, is recommended to bring levels back down. Lifestyle changes also play a big role. Staying active, exercising regularly, avoiding smoking, and keeping hydrated all help keep blood flowing smoothly. In special cases, blood thinners or other medications may be used, but this is usually reserved for men with very high risk.
The U.S. Food and Drug Administration (FDA) has issued warnings about TRT and the chance of blood clots. Medical groups such as the Endocrine Society and the American Urological Association also provide guidance. They recommend that TRT should only be prescribed to men with clearly proven low testosterone and not for general “anti-aging” purposes. They also stress the need for follow-up visits, regular blood tests, and open discussion between doctor and patient. Even though research is still developing, the general advice is to balance benefits against risks on a case-by-case basis.
For patients, this means that open communication with doctors is key. Before starting TRT, it is important to ask: Am I at higher risk for blood clots? How often will my blood be tested? What symptoms should I watch for? What lifestyle changes can lower my risks? These conversations make treatment safer and help avoid serious complications.
In summary, testosterone replacement therapy has the power to improve quality of life for many men with low hormone levels, but it also carries the potential risk of blood clots. The risk does not affect everyone in the same way. It depends on personal health history, method of therapy, and how carefully treatment is monitored. The good news is that with regular testing, smart lifestyle choices, and close guidance from doctors, many risks can be managed. Patients who understand both the benefits and the dangers are in the best position to make safe and informed decisions about their health.
Questions and Answers
Yes, testosterone therapy has been associated with an increased risk of blood clots in some studies, particularly deep vein thrombosis (DVT) and pulmonary embolism (PE). However, the absolute risk appears to be relatively low, and individual factors like age, lifestyle, and medical history also play a role.
Testosterone can increase red blood cell production (erythrocytosis), which makes the blood thicker. This higher viscosity can raise the chance of clot formation in susceptible individuals.
People with a history of blood clots, inherited clotting disorders (like Factor V Leiden), obesity, smoking habits, or prolonged immobility are at higher risk. Older men and those with high hematocrit levels should also be monitored closely.
Blood clots can occur within weeks to months of beginning therapy, though the risk may persist as long as treatment continues, especially if blood counts rise significantly.
Injectable testosterone may cause more rapid increases in red blood cell levels compared to topical gels or patches, potentially increasing clot risk. However, the evidence is mixed, and monitoring is important regardless of the form.
Symptoms include swelling, pain, or redness in the leg (DVT), sudden chest pain, shortness of breath, or coughing up blood (PE). Any of these require urgent medical evaluation.
Yes. Checking hematocrit and hemoglobin levels every 3–6 months helps ensure they stay within safe ranges. If levels get too high, dosage adjustments, switching therapy type, or therapeutic phlebotomy may be recommended.
They should seek emergency medical care immediately. Blood clots can be life-threatening, and early treatment with anticoagulants is critical.
Yes. Medical guidelines recommend avoiding testosterone in men with recent clotting events, uncontrolled high hematocrit, or untreated sleep apnea. Doctors also stress lifestyle management—staying active, avoiding smoking, and controlling weight.
In most cases, yes. Testosterone therapy is generally contraindicated in men with a personal history of blood clots unless a specialist carefully evaluates and manages the risks. Alternative treatments for low testosterone may be safer.