TRT and Fertility: How Testosterone Replacement Impacts Sperm Count and What You Can Do About It
Introduction: Why TRT and Fertility Matter
Testosterone Replacement Therapy (TRT) has become much more common over the past decade. More men are being diagnosed with low testosterone, and many are turning to TRT to help improve mood, energy, strength, sex drive, and overall well-being. Because TRT can offer real benefits for people with confirmed low testosterone, it is easy to see why interest continues to grow. At the same time, more men are choosing to have children later in life, which makes questions about fertility more important than ever. As a result, many people want to know how TRT affects sperm count and whether it can make it harder to have children in the future.
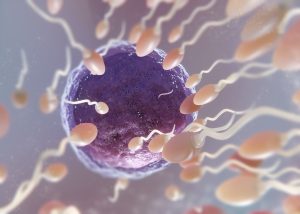
This article focuses on one key topic: how TRT impacts fertility, especially sperm count, and what steps someone can take if they need hormone treatment but also want to protect their ability to have children. Understanding this relationship is important because the effects of TRT on the body are not always obvious. When people hear “testosterone,” they often assume that raising testosterone levels should improve all male reproductive functions. It seems logical that more testosterone would lead to more sperm. However, this is not how the body works. Natural testosterone and medical testosterone behave differently inside the body, and these differences play a major role in fertility.
Before someone starts TRT, it helps to know why testosterone is so closely linked to sperm production. In the male reproductive system, the brain and the testicles work together through a communication loop called the hypothalamic-pituitary-gonadal (HPG) axis. When the brain senses that the body needs more testosterone or more sperm, it sends out signals in the form of hormones. These hormones travel to the testicles and tell them to make both testosterone and sperm. This natural system keeps hormone levels balanced and keeps sperm production steady. When TRT is introduced, this balance can change, and sperm production may slow down or stop entirely. Many people do not expect this because blood testosterone levels may go up while sperm levels go down at the same time.
Because of this, more men are now searching online for answers to basic but important questions: Can TRT cause infertility? Will sperm count go back to normal after stopping TRT? Are the effects permanent? How long does recovery take? Does the type of TRT make a difference? These concerns often appear after someone starts therapy and learns that their fertility may be affected. In some cases, people only discover this after having trouble conceiving, which can create stress, confusion, and frustration.
This article is designed to bring clarity to these questions using clear language and evidence-based information. It explains how natural testosterone supports sperm production, how TRT alters hormone signals, and why sperm count often drops when someone is on therapy. It also reviews current medical knowledge on how quickly these changes occur, how reversible they are, and what steps can help protect fertility while still treating low testosterone. Some men may be able to support sperm production with additional medications. Others may choose to store sperm before treatment begins. Understanding these options early can make a big difference in long-term family planning.
The goal of this article is not to discourage TRT. Instead, it aims to help people make informed decisions. With the right guidance, it is possible to treat low testosterone while reducing the impact on fertility. By learning how TRT interacts with the body’s natural systems, readers can have better conversations with their healthcare providers, ask stronger questions, and plan their treatment in a way that keeps both health and future goals in mind.
As you move through the next sections, you will learn exactly how sperm production works, why TRT affects it, and what practical steps can help maintain fertility during treatment. The information is written in simple, easy-to-understand language so every reader can feel confident and informed, no matter their medical background.
How Natural Testosterone Regulates Sperm Production
To understand how testosterone replacement therapy (TRT) affects sperm count, it is important to first understand how the body normally makes testosterone and sperm. The male reproductive system works through a careful communication loop called the hypothalamic-pituitary-gonadal (HPG) axis. This system makes sure the body produces the right amount of hormones to support both sexual health and fertility. When this loop is working correctly, the testicles produce natural testosterone and healthy sperm in steady amounts. When the loop is disrupted, sperm production can drop.
The HPG Axis: The Body’s Hormone Control Center
The HPG axis is made of three main parts:
- The hypothalamus – a small area in the brain
- The pituitary gland – a tiny gland under the brain
- The testes – the organs that make testosterone and sperm
These three parts communicate like steps in a chain.
Step 1: The Hypothalamus Signals the Pituitary Gland
The process begins in the hypothalamus. It releases a hormone called GnRH (gonadotropin-releasing hormone). GnRH acts like a “messenger signal” that tells the pituitary gland to release more hormones. This signal comes in pulses throughout the day, which keeps the system working at a normal rhythm.
Step 2: The Pituitary Gland Releases LH and FSH
When the pituitary gland receives the GnRH signal, it releases two very important hormones:
- LH (luteinizing hormone)
- FSH (follicle-stimulating hormone)
Each hormone has its own job in the testicles.
LH tells the testicles to produce testosterone.
FSH tells the testicles to support sperm cell development.
Both hormones are needed to keep sperm production strong.
Step 3: The Testicles Produce Testosterone and Sperm
Inside the testicles, there are two main types of cells that respond to LH and FSH:
- Leydig cells – these make testosterone when they receive LH
- Sertoli cells – these help grow and mature sperm when they receive FSH
Together, these cells create the ideal environment for making sperm.
The Importance of Intratesticular Testosterone
When people think about testosterone, they often think about the level measured in a blood test. But for sperm production, the most important testosterone level is the amount inside the testicles, not in the bloodstream.
This is called intratesticular testosterone (ITT).
ITT levels must be much higher than the levels found in normal blood tests—often up to 100 times higher. These high levels inside the testes are necessary because developing sperm cells need a strong and steady supply of testosterone to grow properly.
If ITT drops, sperm production slows down or may stop completely.
How Spermatogenesis Works
Spermatogenesis is the process of making sperm. It takes about 64–72 days for a sperm cell to fully develop. During this time, each sperm cell must go through several stages:
- Early cell division
- Growth and shaping
- Development of the tail
- Final maturation in the epididymis
This long process depends on stable hormonal support. Testosterone and FSH help guide immature cells through each stage. If hormone levels drop, sperm cells may not mature correctly. This can affect:
- Sperm count
- Sperm movement (motility)
- Sperm shape (morphology)
Because the process takes several weeks, any change in hormone levels may affect sperm health months later.
How the Body Maintains Balance
The HPG axis works through a system called negative feedback. When your testicles make enough testosterone, the brain senses it and reduces how much GnRH, LH, and FSH it releases. This prevents testosterone from becoming too high.
In a natural system, this balance keeps hormones stable and supports sperm production.
Why This Matters for TRT
Understanding this natural system is key to understanding why TRT affects fertility. When testosterone is supplied from outside the body—as a gel, injection, or patch—the brain senses high testosterone in the blood. It then reduces GnRH, LH, and FSH production. Without LH and FSH signals, the testicles stop producing intratesticular testosterone, which is required for sperm production.
What TRT Is and Why It’s Prescribed
Testosterone Replacement Therapy, often called TRT, is a medical treatment used to raise testosterone levels in people who have low testosterone. Testosterone is a hormone made mostly in the testes. It plays a major role in energy, muscle strength, mood, sexual health, and overall well-being. When the body cannot make enough testosterone on its own, symptoms can appear that affect daily life. TRT is one of the main treatments doctors use to bring testosterone levels back to a healthy range.
What “Low Testosterone” Means
Low testosterone—sometimes called hypogonadism—is a medical condition where the testes do not make enough testosterone. This can happen for many different reasons. Some people are born with conditions that affect hormone production. Others develop low testosterone after injury, surgery, illness, or due to aging. Some medications can also lower testosterone.
Common symptoms include:
- Fatigue
- Lower sex drive
- Erectile difficulties
- Loss of muscle mass or strength
- Mood changes
- Difficulty concentrating
- Loss of body hair
Doctors confirm low testosterone with blood tests, usually done in the early morning when levels are highest.
Why TRT Is Prescribed
Doctors prescribe TRT to treat confirmed low testosterone when symptoms are significant and affect quality of life. The goal is to restore testosterone to a normal range—not to raise it above normal levels.
TRT can help:
- Improve energy levels
- Increase libido
- Support erections
- Increase muscle strength
- Improve bone density
- Improve mood and mental clarity
It’s important to understand that TRT is a medical treatment, not a performance-enhancing shortcut. Doctors only prescribe it when clear medical needs are present.
Who May Need TRT
Not everyone with mild symptoms needs TRT. Doctors look at both symptoms and hormone levels before making a diagnosis. People who may need TRT include those with:
- Primary hypogonadism (testes do not make testosterone)
- Secondary hypogonadism (brain does not send the signals needed to produce testosterone)
- Testicular injury or removal
- Genetic disorders affecting testosterone production
- Some pituitary gland disorders
- Long-term opioid use
- Certain chronic illnesses that reduce hormone production
In many of these cases, testosterone levels stay low even after treating underlying conditions. For these individuals, TRT provides a long-term way to restore hormone levels.
Different Forms of TRT
TRT comes in several forms. Each delivers testosterone into the body in a different way, and each has benefits and drawbacks.
Injections
Testosterone injections are one of the most common forms of TRT. They are usually given every 1–2 weeks, or sometimes weekly, depending on the dose and the type of testosterone used.
Advantages:
- Predictable dose
- Lower cost
- Long history of use
Disadvantages:
- Levels may rise and fall between doses
- Requires needles or clinic visits
Gels
Hormone gels are applied to the skin once each day. Testosterone absorbs through the skin into the bloodstream.
Advantages:
- Steady hormone levels
- Easy to use
Disadvantages:
- Must avoid skin contact with others until dry
- Can be expensive
Patches
Testosterone patches attach to the skin and release hormone slowly over 24 hours.
Advantages:
- Consistent absorption
- Simple daily routine
Disadvantages:
- Skin irritation is common
Pellets
Testosterone pellets are placed under the skin by a healthcare provider. They release hormone slowly for 3–6 months.
Advantages:
- No daily dosing
- Very stable levels
Disadvantages:
- Requires a minor procedure
- Dose cannot be adjusted until pellets dissolve
How Therapeutic Testosterone Differs From Natural Testosterone
Understanding the difference between natural testosterone and therapeutic testosterone is important, especially for fertility.
Your testes normally produce testosterone only when the brain sends signals through hormones called LH (luteinizing hormone) and FSH (follicle-stimulating hormone). These hormones are part of the hypothalamic-pituitary-gonadal (HPG) axis, which regulates both testosterone production and sperm production.
When you take TRT, the body senses that testosterone levels in the blood are high. This causes the brain to reduce LH and FSH signals. When these signals drop, the testes slow down or stop producing testosterone on their own. This includes the intratesticular testosterone needed for healthy sperm production.
This is why TRT can strongly affect fertility, even when blood testosterone levels look healthy.
Why Understanding TRT Is Important Before Starting
Before beginning TRT, it’s important to know:
- It supports testosterone levels in the blood
- It does not restore sperm production
- It may reduce or stop natural testosterone and sperm production
- It can require long-term treatment
Some people think TRT boosts all forms of testosterone, but this is not correct. TRT increases circulating testosterone but may lower the testosterone inside the testes, which is key for fertility. Understanding this difference is important for anyone who may want biological children in the future.
How TRT Affects Sperm Count: The Biological Mechanisms
Testosterone Replacement Therapy (TRT) can have a strong effect on fertility because it changes how the body controls hormone levels inside the testes. Even though TRT raises testosterone in the bloodstream, it often lowers the testosterone level inside the testes, which is the level that truly matters for sperm production. Understanding this difference is key to understanding why sperm count can fall during TRT.
This section explains the hormonal pathways involved, why they become suppressed, and how this leads to lower sperm count, changes in sperm quality, and in some cases, complete temporary loss of sperm (azoospermia).
How TRT Suppresses the Hormone Signals From the Brain
Sperm production depends on a communication loop between the brain and the testes called the hypothalamic–pituitary–gonadal (HPG) axis. Here is how the system works under normal conditions:
- The hypothalamus releases a hormone called GnRH.
- The pituitary gland responds by releasing two more hormones:
- LH (luteinizing hormone)
- FSH (follicle-stimulating hormone)
- LH tells the testes to make testosterone inside the testicles (intratesticular testosterone).
- FSH helps support the cells that make sperm.
This system stays balanced through “feedback.” When testosterone levels rise or fall, the brain adjusts how much GnRH, LH, and FSH it sends out.
When a person starts TRT, the external testosterone raises levels in the blood. The brain reads this as “testosterone is high enough.” As a result, the brain sends a message to slow down GnRH, LH, and FSH production. When LH and FSH drop, the testes no longer receive the signals they need to produce testosterone inside the testicles or to continue strong sperm production.
This is why many people on TRT have normal or even high blood testosterone, but low sperm count.
Decline in Intratesticular Testosterone
TRT replaces testosterone in the bloodstream, but it does not replace testosterone inside the testes. For healthy sperm to grow, intratesticular testosterone needs to be much higher than the testosterone circulating in the blood—often 50–100 times higher.
When TRT shuts down LH, the cells in the testes stop producing this very high, local testosterone. Even if a blood test shows strong “T levels,” the actual testosterone inside the testicles may become too low to support sperm development.
This drop in intratesticular testosterone is one of the main reasons sperm count declines during TRT.
Impact on Sperm Count
With less LH and FSH and low intratesticular testosterone, the testes cannot keep producing sperm at normal levels. The effects can include:
- Reduced sperm count: This is the most common effect.
- Severely low sperm count (oligospermia): Sperm numbers may fall far below the normal range.
- Complete absence of sperm (azoospermia): Some individuals produce no measurable sperm while on TRT.
The amount of reduction depends on factors such as age, dose of TRT, sensitivity to hormones, and how long the therapy has been used.
Impact on Sperm Motility and Morphology
TRT can also affect sperm quality, not just quantity.
Motility
Motility refers to how well sperm move. Lower intratesticular testosterone can weaken the environment in which sperm mature. This may result in sperm that swim more slowly or less effectively.
Morphology
Morphology describes the shape of sperm. Hormonal suppression can affect how sperm form inside the testes, increasing the chance of abnormal shapes, which may reduce the ability to fertilize an egg.
Why TRT Can Lead to Temporary Azoospermia
In some cases, TRT suppresses the HPG axis so strongly that sperm production stops almost completely. This is known as azoospermia. It is often temporary when TRT is stopped, but the recovery time varies widely. Some people see their sperm return within a few months, while others need a year or longer.
This effect is not rare. Studies have shown that a significant percentage of men using TRT experience very low sperm counts, and many reach azoospermia during treatment.
TRT raises testosterone in the blood but shuts down the brain’s natural hormone signals that support sperm production. Without LH and FSH, the testes cannot maintain the high intratesticular testosterone levels needed for healthy sperm. This leads to lower sperm count, weaker sperm movement, and changes in sperm shape. In some individuals, sperm production may stop entirely while on TRT.
This mechanism is important to understand for anyone who may want biological children in the future, as it explains why planning fertility before starting TRT is so important.
How Quickly TRT Impacts Sperm Count
Testosterone Replacement Therapy (TRT) can have a strong impact on the body’s natural hormones. One of the first systems affected is the hypothalamic-pituitary-gonadal (HPG) axis, which controls sperm production. Understanding how quickly these changes happen is important for anyone who wants to protect their fertility while using testosterone.
How the HPG Axis Responds to TRT
The HPG axis includes the brain and the testes. In healthy men, this system works like a feedback loop:
- The brain releases GnRH (gonadotropin-releasing hormone).
- GnRH tells the pituitary gland to release LH (luteinizing hormone) and FSH (follicle-stimulating hormone).
- LH signals the testes to make testosterone.
- FSH supports the cells that help produce sperm.
When you start TRT, the body senses that testosterone levels in the blood are rising. Because of this, the brain tries to “balance” the hormones by turning down the release of GnRH, LH, and FSH.
When LH and FSH fall, sperm production slows down.
This internal shift can happen quickly, which is why fertility changes can appear early in treatment.
When Sperm Count Starts to Drop
Most studies show that sperm count begins to fall within a few weeks to a few months after starting TRT. The timeline depends on several factors, including the dose, the form of TRT used, and the person’s natural hormone levels.
Typical timeline:
- Weeks 2–6:
LH and FSH levels begin to drop sharply. The testes receive fewer signals to produce sperm. Some men may notice early changes such as smaller testicular size or a feeling of “tightness,” although these signs are not always obvious. - Weeks 6–12:
Intratesticular testosterone (testosterone inside the testes) drops. Even though blood testosterone levels are high, the testes no longer receive the signal needed to make testosterone locally. Because intratesticular testosterone must stay extremely high for sperm development, this decline causes a significant slowdown in sperm production. - Months 3–6:
Many men show a marked drop in sperm count. Some reach very low levels or even azoospermia (no measurable sperm in the semen). This is temporary for most men, but it is a clear sign of strong hormonal suppression. - Months 6–12:
With continued TRT, sperm production may remain very low. The longer this suppression lasts, the more time recovery may take if TRT is stopped later.
Why Intratesticular Testosterone Matters for Timing
A key part of understanding the timing is knowing that sperm production depends on very high testosterone levels inside the testes—much higher than the levels seen in the bloodstream.
TRT raises testosterone in the blood but lowers testosterone inside the testes. This is because the testes stop receiving LH, which they need to make their own supply.
This decrease begins early and creates the conditions for sperm production to slow down in the first several weeks.
Do All Men Experience a Fast Drop in Sperm Count?
Not every man will have the same response, because hormone levels and testicular sensitivity are different from person to person. But clinical data show several general patterns:
Men who may see faster suppression:
- Those on higher TRT doses
- Those using long-acting injections or pellets
- Younger men with strong baseline hormone activity
- Men who already have low LH and FSH levels before starting TRT
Men who may see slower suppression:
- Those on low-dose TRT
- Those using gels or patches
- Men who naturally have slower hormonal responses
- Men taking medications that support LH/FSH
Even with these differences, the majority of men on TRT will show some degree of sperm suppression within the first few months.
How Doctors Track These Changes
Healthcare professionals may monitor changes with:
- Semen analysis (to check sperm count and quality)
- Blood tests (to measure testosterone, LH, and FSH)
- Physical exam (to check testicular size and other signs)
Monitoring is especially important for people who plan to have children in the future.
TRT can begin to reduce sperm count within weeks, with more noticeable changes usually appearing between 2 and 3 months. By 6 months, many men experience significant suppression. These effects are typically reversible once TRT is stopped, but the timeline varies from person to person.
Reversibility: What Happens When You Stop TRT
One of the biggest questions people have about testosterone replacement therapy (TRT) is whether sperm production can return after stopping treatment. This is an important concern for anyone who may want children in the future. The good news is that fertility often comes back for many men once TRT is stopped. But recovery is not instant. It depends on several factors, such as age, how long TRT was used, and overall reproductive health. This section explains what happens inside the body, how long recovery may take, and what science shows about typical timelines.
What Happens to Hormones When TRT Stops
To understand recovery, it helps to know how TRT changes the body. When a person uses TRT, the brain senses the high testosterone levels in the bloodstream. As a result, it reduces or stops sending signals to the testes to make testosterone. These signals are two hormones called luteinizing hormone (LH) and follicle-stimulating hormone (FSH). Both are needed for sperm production.
When TRT is stopped, the brain needs time to “turn back on” these signals. At first, LH and FSH remain low, so sperm production stays low. Slowly, the hypothalamic-pituitary-gonadal (HPG) axis begins to recover. Over weeks to months, LH and FSH levels rise again, and the testes start producing testosterone and sperm at higher levels.
This process does not happen overnight. It usually takes several months for hormone levels to improve and for sperm production to resume.
Typical Timelines for Sperm Count Recovery
Recovery time varies from person to person, but research provides general patterns. Many studies show that most men see sperm production return to normal within 3 to 12 months after stopping TRT. Some men recover faster, while others take longer.
Here are the typical stages:
First 1 to 3 Months: Early Hormone Changes
- LH and FSH begin rising again as the brain restarts the signals needed for sperm production.
- Blood testosterone levels may go down before they stabilize.
- Most men do not see a rise in sperm count yet, because sperm take about 64–72 days to develop.
Months 3 to 6: Beginning of Measurable Recovery
- The testes respond to the rising LH and FSH.
- Intratesticular testosterone levels increase, which is necessary for sperm development.
- Many men begin to see improvement in sperm count during this period.
Months 6 to 12: Significant Recovery
- For many men, sperm counts return to the normal range within this timeframe.
- Motility and morphology often improve as well.
- Hormone levels typically stabilize, though some men may still show fluctuations.
Beyond 12 Months: Delayed Recovery
- A small percentage of men take longer than a year to return to normal sperm levels.
- Delayed recovery is more common in men who used TRT for many years or who are older.
- Recovery is still possible, but it requires more time and medical monitoring.
Factors That Affect Recovery Speed
Not everyone recovers at the same rate. Several factors play a role:
Age
Younger men usually recover faster because their testes and hormone pathways are more responsive. Older men may take longer because natural hormone levels decline with age, making recovery slower.
Duration of TRT Use
Short-term use (less than a year) is linked with quicker recovery. Long-term use may cause deeper suppression of hormone signals, which means the body needs more time to rebuild sperm production.
Baseline Fertility
Men who had normal sperm counts before TRT usually recover more easily. Men with fertility issues before starting TRT may take longer or require medical help to recover.
Underlying Health Conditions
Diseases such as pituitary disorders, testicular injury, or metabolic issues can slow recovery. These conditions may interfere with the HPG axis, making natural testosterone and sperm production harder to regenerate.
Type of TRT
Some TRT methods cause more suppression than others. For example, injections often create high peaks of testosterone in the blood, which may cause stronger suppression. Gels and patches may have a gentler impact. The method used can affect how long recovery takes.
What Research Shows About Recovery
Studies on men recovering from TRT or testosterone-based male contraceptive trials show that most regain normal sperm counts within a year. These studies help predict recovery because the hormonal changes are similar to what happens during and after TRT.
Key findings include:
- Most men recover to at least 20 million sperm per milliliter (a common marker of normal fertility) within 3–6 months.
- Nearly all men recover normal sperm levels within 12 months.
- A small group may take up to 24 months, especially after long-term use.
These timelines show that recovery is common, but not always fast.
When Medical Support May Be Needed
Some men may need medication to help restart sperm production. Doctors sometimes prescribe medicines that stimulate LH and FSH production if natural recovery is slow. These treatments can speed up sperm return and support overall hormone balance. While this article does not give medical advice, it is important to know that slow recovery is not unusual and often treatable.
Stopping TRT allows the body to gradually restart natural hormone production. For many men, sperm counts recover within 3 to 12 months, while others may take longer depending on age, TRT duration, and baseline fertility. Recovery is common, but it requires time, patience, and sometimes medical support. Understanding the process can help men make informed decisions about fertility planning when considering or discontinuing TRT.
Fertility-Preserving Strategies for Men Who Need Testosterone Support
Many men want the benefits of testosterone therapy but still wish to protect their ability to have children. This can feel confusing, because traditional testosterone replacement therapy (TRT) can lower sperm production. However, there are medical strategies that can help keep the testicles active and maintain, or support, sperm development while treating low testosterone. This section explains these strategies in clear detail, so readers understand how they work and why doctors may use them.
Understanding Why Fertility Support Is Needed During TRT
Before talking about specific treatments, it helps to understand why fertility support is needed in the first place. When someone takes testosterone from an outside source—like injections, gels, or pellets—the brain senses the higher level of testosterone in the bloodstream. It then slows or stops the release of two key hormones: luteinizing hormone (LH) and follicle-stimulating hormone (FSH).
These hormones tell the testicles to do two important jobs:
- LH helps the testicles make testosterone inside the testes.
This local testosterone level must be very high to support sperm development. - FSH helps the testicles create and mature sperm cells.
When LH and FSH drop, sperm production slows down or stops. That is why many men on TRT develop very low sperm counts. Fertility-preserving strategies aim to keep LH and FSH working, or to replace their effects, so the testicles stay active.
Medical Therapies Used to Support or Maintain Sperm Production
There are several medical options doctors use to help protect fertility while someone is taking testosterone or treating low testosterone. These are not simple over-the-counter solutions. They are prescription treatments managed by healthcare professionals who monitor hormone levels and sperm health over time.
Therapies That Stimulate LH and FSH Production
Some medications cause the body to release more LH and FSH. These therapies do not replace testosterone. Instead, they tell the brain to restart signals that stimulate the testicles. By doing this, they help keep sperm production going even when testosterone levels are being adjusted or supported.
This approach is helpful when someone wants to improve testosterone symptoms but also wants to stay fertile or avoid a major drop in sperm count.
Therapies That Act Like LH to Support the Testicles
Another set of treatments works by taking the place of LH. These therapies provide a signal that “turns on” the testicles, even when the brain has reduced natural LH. This helps the testicles continue making the high level of internal testosterone needed for sperm development.
This strategy is often used in men who want the physical and mental benefits of better testosterone levels, but who also want their testicles to keep functioning normally.
Therapies Involving Hormones That Directly Support Sperm Development
Some treatments are used to mimic the effects of FSH. These therapies are often recommended when sperm counts are already very low or when a couple is trying to conceive within a specific timeframe. These options are usually part of a treatment plan guided by fertility specialists and may involve regular sperm testing and hormone tracking.
How Doctors Decide Which Fertility Strategy to Use
No single treatment works for everyone. Doctors make choices based on several factors, including:
- The patient’s age
- Current sperm count
- Severity of low testosterone
- How long the person has been on TRT
- Plans for conceiving soon or in the future
- Other medical conditions that may affect fertility
Because each patient’s situation is different, hormone levels must be checked regularly. This may include blood tests, semen analysis, and questions about symptoms over time.
Monitoring Sperm Health During Treatment
Monitoring is a key part of keeping fertility safe. Doctors often use:
- Blood tests to check testosterone, LH, FSH, and other hormone levels
- Semen analysis to measure sperm count, movement, and shape
- Regular check-ins to discuss symptoms and make sure treatment is working
Monitoring lets doctors adjust medication doses, change therapy plans, or pause certain treatments when needed.
Working With a Professional Is Essential
Because fertility preservation involves hormone-based medicine, it must be supervised by a qualified healthcare professional. Self-treatment or guessing doses can lead to long-term fertility problems or unsafe hormone levels. A medical expert will help balance two goals at the same time: improving testosterone levels and protecting the ability to have children.
Special Considerations for Different TRT Delivery Methods
Testosterone replacement therapy (TRT) can be given in several different forms, and each method affects the body in a unique way. While every type of TRT can lower sperm production, the speed, degree, and pattern of this effect can vary. Understanding how each method works can help men make more informed choices, especially if they are concerned about fertility. Below is a detailed look at how injections, gels, patches, and pellets influence hormone levels and how these changes may impact sperm count.
Injections
Testosterone injections are one of the most common forms of TRT. They are usually given every one to two weeks for short-acting versions and every 10 to 14 weeks for long-acting versions. Injections deliver testosterone directly into the muscle, where it enters the bloodstream and causes a fast rise in testosterone levels.
This rapid increase can create very high peaks of testosterone shortly after the shot. These peaks can strongly suppress the body’s natural release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). When LH and FSH are suppressed, the testes produce less intratesticular testosterone, which is the form of testosterone needed to make sperm. Because of this sharp suppression, injections often have one of the strongest and quickest effects on sperm count.
Short-acting injections may cause more dramatic hormone swings compared to long-acting ones. The larger the peak after each shot, the more the brain reduces its own hormone signals. Over time, this can lead to a deep drop in sperm production, and in some cases, complete temporary absence of sperm (azoospermia). Many studies show that injectable testosterone is among the most likely TRT forms to reduce sperm count rapidly.
Gels
Testosterone gels are applied to the skin once a day. They provide a steady and controlled release of testosterone into the bloodstream. This method tends to cause more stable hormone levels, without dramatic peaks or drops.
Because gels produce smoother and more even testosterone levels, some people assume they might have a smaller effect on fertility. However, this is not always true. Even though hormone peaks are not as sharp as injections, the overall rise in testosterone is still enough to reduce LH and FSH. Over time, this suppression can still lower intratesticular testosterone, which can reduce sperm count.
Gels can also vary in how much testosterone each person absorbs. Some people absorb more than others, which means their sperm suppression may be stronger. Others absorb less, which may lead to milder suppression. But even with these differences, testosterone gels still carry a significant risk of lowering sperm production, and men who want children should be aware of this.
Patches
Testosterone patches work similarly to gels. They release testosterone through the skin and keep hormone levels fairly steady. Patches usually produce lower peaks than injections and may have more predictable absorption than gels.
While the hormonal effect from patches may seem moderate, the body still senses the increase in testosterone. This leads to reduced signaling from the brain and less production of LH and FSH. As a result, sperm production can still fall. The timeline may be slower compared to injections, but patches still carry a meaningful risk of reducing fertility.
Some men prefer patches because they avoid daily application of gel and avoid sharp hormonal spikes. However, when it comes to fertility, patches should be considered similar to other forms of TRT: they can suppress sperm production and should be used carefully if future fertility is important.
Pellets
Testosterone pellets are placed under the skin, usually in the hip area. They release testosterone slowly over three to six months. Because pellets provide a long-term, steady release, they avoid the large hormone peaks seen with injections. However, they also cannot be easily adjusted or stopped once inserted.
This long-lasting release leads to consistent suppression of the body’s own hormone signals. Pellets can reduce LH and FSH for the entire time they are active. Because the treatment cannot be reversed until the pellets dissolve, the suppression of sperm production may last longer than with gels or patches. This can be a challenge for men who may want to restore fertility quickly.
Pellets can be convenient, but they often lead to long-lasting suppression of sperm production due to their continuous nature and long duration of action.
Which Method Affects Fertility the Most?
All forms of TRT can reduce sperm count, but the pattern differs:
- Injections: strongest peaks, often fastest suppression
- Pellets: long-lasting suppression without easy reversal
- Gels and patches: smoother levels but still significant suppression over time
No method is “safe” for fertility. Any external testosterone can lower intratesticular testosterone, which is the key hormone needed for sperm production.
Why the Delivery Method Matters
The delivery method matters because it affects how quickly testosterone levels rise, how steady they stay, and how long the hormone remains active. The more consistently blood testosterone is elevated, the more the brain reduces its own hormone production. This means less LH and FSH, and therefore less sperm production.
For men who want to preserve fertility, it is important to understand these differences and discuss them with a healthcare professional before choosing a TRT method.
TRT, Age, and Overall Reproductive Health
Age plays a major role in how the body responds to testosterone replacement therapy (TRT). While TRT can help improve energy, mood, and sexual function, its effects on fertility can change depending on how old a person is and what stage of life they are in. Understanding these differences is important for anyone who is thinking about TRT and also wants to protect or plan for future fertility.
This section explains how age affects testosterone levels, sperm production, and how the body responds to TRT. It also covers what younger and older patients should consider before starting treatment.
How Age Influences Hormonal Patterns
Natural testosterone levels change over time. For most people, testosterone peaks in the late teen years and early 20s. After about age 30, testosterone slowly drops each year. This decline is normal and expected, but the amount and speed of decline vary from one person to another.
Younger people usually have stronger signals from the brain to the testes through the hypothalamic-pituitary-gonadal (HPG) axis. This means their bodies are more sensitive to changes in hormones. Because of this, when a young person starts TRT, the suppression of the HPG axis can be more noticeable. The brain senses the higher testosterone levels in the bloodstream from TRT and reduces the release of LH and FSH. These two hormones are needed for sperm production, so shutting them down can cause sperm counts to fall quickly.
For older adults, the HPG axis may already be weaker due to age. Their natural testosterone may have been low for years, and the signaling between the brain and testes may be less active. In these cases, TRT can still lower LH and FSH, but the overall impact might feel different because their sperm production may already be reduced before starting treatment.
Fertility Considerations for Younger vs. Older Patients
Younger Adults
People in their 20s or early 30s often have the highest natural fertility. Their sperm counts are usually strong, and they may have future plans to build a family. Because TRT can significantly reduce sperm production, younger adults should take special care before beginning therapy.
Key points for younger patients include:
- Higher risk of full suppression: TRT can quickly shut down sperm production, and in some cases lead to temporary azoospermia (no sperm).
- Longer recovery time: Younger men often recover fertility well after stopping TRT, but it may still take months or longer.
- Planning ahead: Anyone who may want children later should talk with a healthcare professional about preserving fertility, such as sperm banking or using medications that protect sperm production.
Middle-Aged Adults
People in their late 30s to 50s may notice more symptoms of low testosterone, including fatigue, reduced sex drive, and changes in body composition. Some are also at a stage of life where family planning is complete. Still, many individuals in this age group do want to maintain fertility.
Key points for middle-aged patients include:
- Moderate risk of suppression: TRT continues to reduce LH and FSH at any age.
- Baseline fertility may already be lower: Age-related changes, lifestyle, and medical conditions can affect fertility before TRT even begins.
- Shared decision-making: A fertility discussion with a clinician can help clarify priorities and guide treatment choices.
Older Adults
People over 50 often use TRT for symptom relief or medical reasons. Fertility is usually less of a concern in this age group, but it is still important to understand how TRT affects reproductive health.
Key points for older patients include:
- Age-related sperm decline: Sperm count, sperm quality, and hormone levels often drop with age, sometimes making the effects of TRT harder to separate from natural aging.
- TRT may not change fertility goals: Many older adults no longer plan to have children, so the impact on sperm production may be less important.
- Monitoring still matters: Even when fertility is not a priority, hormone levels and testicular health should be monitored.
Sexual Function Improvements vs. Fertility Concerns
One common point of confusion is the difference between sexual function and fertility. TRT often improves sexual desire, energy, erections, and mood. Because of this, some people believe it should also boost fertility. However, these two areas are controlled by different processes in the body.
Sexual function improves with higher blood testosterone.
Fertility depends on high testosterone inside the testes and strong signals from LH and FSH.
These systems do not always rise and fall together. TRT can improve sex drive while lowering sperm production at the same time. Understanding this difference helps set realistic expectations and prevents misunderstandings.
Age strongly affects how the body responds to TRT and how fertility changes over time. Younger people often have more to lose when TRT suppresses sperm production, while older people may see less impact because their fertility is already reduced. Regardless of age, it is important to talk with a healthcare professional, review the benefits and risks, and decide on a plan that supports both hormone health and long-term reproductive goals.
Conclusion: Making Informed Decisions About TRT and Fertility
Testosterone replacement therapy can be life-changing for men who struggle with low testosterone, but it is important to understand that it can also affect fertility in significant ways. Many people start TRT for symptoms like fatigue, low sex drive, trouble concentrating, or decreased muscle strength, without realizing that the therapy can lower or even stop sperm production. This happens because the body responds to outside testosterone by reducing the natural signals that tell the testes to make both testosterone and sperm. Even though blood testosterone levels rise with TRT, the levels inside the testes fall, and sperm development depends on high levels inside the testes. This difference explains why a man can feel better on TRT yet see a drop in sperm count at the same time.
Understanding this process helps make sense of why fertility can change during treatment and what can be done about it. Some people assume that TRT affects sperm count the same way for everyone, but this is not true. The impact depends on several factors, like the dose of testosterone, how long someone has been on therapy, the delivery method used, and the person’s age and baseline fertility. In many cases, TRT can lower sperm count within a few months. In some individuals, sperm count may fall to very low levels or become temporarily absent. This can be alarming if someone hopes to start or grow a family, which is why planning and early conversations are so important.
The good news is that fertility often improves after stopping TRT, but recovery time is different for everyone. For many, sperm levels begin to rise within months, but full recovery can take longer. Age plays a strong role because younger men tend to regain fertility faster than older men. How long someone has been on TRT also matters. Short-term use is more likely to lead to quick recovery, while long-term use may require more time. Even so, most men do see improvement once treatment stops because the body begins to restart its natural hormone signals.
For those who need testosterone support but also want to protect their fertility, options exist. Some medical treatments can help maintain sperm production while a person is on TRT. These treatments work by stimulating the body’s own hormone signals so the testes keep producing sperm. Not everyone is a candidate for these treatments, and they must be prescribed and monitored by a qualified healthcare professional. Because every individual’s hormone system is different, the right plan needs careful evaluation, regular testing, and adjustments over time.
Different TRT delivery methods can also influence fertility. Injections may cause large swings in testosterone levels, while gels and patches provide more steady levels. Pellets release testosterone slowly over several months. All forms can affect sperm production, but the speed and degree of suppression may vary. Understanding these differences helps people make informed choices if they need TRT but are also thinking about future fertility. No method is completely “fertility friendly,” but some may be easier to adjust or stop if someone needs to restore natural hormone function.
Communication with a healthcare professional is one of the most important parts of making safe and informed decisions. Patients should feel comfortable asking questions about how TRT might affect their fertility, what changes to expect, and what steps can be taken to protect their reproductive goals. Common tests include hormone panels and semen analyses, which help track how the body is responding to treatment. These tests also guide decisions about whether to adjust therapy or add fertility-supporting medication. Planning ahead offers the best chance of keeping options open, especially for individuals who may want to have children later.
Making informed choices about TRT means weighing the benefits—such as improved energy, mood, and sexual health—against the possible impact on fertility. For many people, understanding these trade-offs reduces uncertainty and helps them feel more confident about their healthcare decisions. This topic is deeply personal, and the right path is different for each person. With clear information, ongoing communication, and medical support, it is possible to find a balance between managing low testosterone and protecting long-term reproductive health.
Questions and Answers
Yes. TRT can significantly lower sperm count because external testosterone suppresses the brain signals (LH and FSH) needed for sperm production.
TRT tells the brain that the body has enough testosterone, which shuts down the testes’ natural testosterone production—something required locally inside the testes to make sperm.
For most men, no. Sperm production often returns within months after stopping TRT, but recovery time varies and is not guaranteed.
Typical recovery is 3–12 months, though some men may take longer depending on dose, duration, and individual biology.
Not significantly. All forms of TRT can suppress sperm production because they all affect the same hormonal feedback loop.
Yes. Drugs like hCG, FSH, or SERMs (e.g., clomiphene) can stimulate the testes to keep producing sperm while on or instead of TRT.
Mostly sperm count, but motility and morphology can also decrease because overall sperm production is suppressed.
Yes. TRT often causes testicular shrinkage because the testes become less active when stimulated less by LH and FSH.
Yes. Young men tend to have stronger hypothalamic–pituitary–testicular (HPT) axis activity, making TRT’s suppressive effects more noticeable.
Yes. Clomiphene, enclomiphene, and hCG-based therapy can raise testosterone levels without directly suppressing sperm production and are often used for men who want fertility preserved.