TRT and Cholesterol: How Testosterone Therapy Really Affects Your Heart Health
Introduction: Why Testosterone Therapy and Cholesterol Are So Closely Linked
Testosterone Replacement Therapy, often called TRT, is a medical treatment used to raise testosterone levels in people who have clinically low hormone levels. Low testosterone can cause fatigue, reduced strength, low mood, and changes in body composition. Because TRT can improve these symptoms, its use has grown in recent years. At the same time, many people have become concerned about how TRT might affect cholesterol levels and heart health. Cholesterol plays a central role in heart disease, so even small changes can feel important to patients who want to protect their long-term health. This makes understanding the connection between TRT and cholesterol an essential topic for anyone considering or already using testosterone therapy.
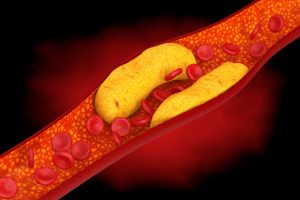
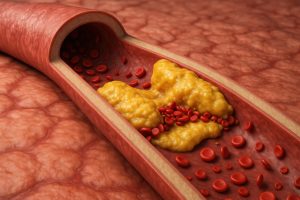
Cholesterol itself is not always harmful. It is a natural substance that the body uses to build cells, make hormones, and support the brain. Problems arise when cholesterol levels become unbalanced, especially if LDL cholesterol—often called “bad cholesterol”—gets too high or if HDL cholesterol—known as “good cholesterol”—gets too low. High LDL increases the risk of plaque building up inside the arteries. When plaque becomes thick or unstable, it can block blood flow or cause a clot, which raises the risk of a heart attack or stroke. Because of this, doctors pay close attention to anything that could shift cholesterol levels, including hormone therapy.
People sometimes worry that TRT might increase their risk of heart problems. This concern often comes from mixed messages online, conflicting research studies, and comparisons between medical TRT and anabolic steroid abuse. These two things are not the same. Medical TRT uses doses that restore normal, healthy hormone levels. Steroid abuse involves extremely high doses far above what the body needs. Because the public often hears these topics discussed together, many people have unanswered questions about how medical TRT truly affects cholesterol and cardiovascular health. The purpose of this article is to give clear, evidence-based information so readers can understand what current research shows.
This article explains how testosterone affects cholesterol, why different people respond differently, and what current medical studies say about heart risk during TRT. It also breaks down the different types of cholesterol and why each type matters. Many people do not realize that testosterone interacts with the liver, fat tissue, inflammation, and blood cells—all of which can influence cholesterol levels. Understanding this connection makes it easier to see why doctors monitor blood tests so closely during TRT.
Another reason this topic matters is that millions of adults already have some form of heart risk. Conditions like obesity, diabetes, high blood pressure, and high cholesterol are common. These conditions can change how the body responds to TRT, and they may also change how safe the therapy is for each individual. Someone with a long history of high LDL may need more frequent monitoring than someone with no cardiovascular risk factors at all. This article explains these differences so that readers can understand what factors they and their doctors should consider before starting treatment.
The goal of this article is not to promote or discourage TRT. Instead, it aims to give readers clear medical information in simple, easy-to-understand language. Many studies have explored how TRT influences cholesterol levels, inflammation, arterial plaque, and overall cardiovascular outcomes. Some studies have shown neutral effects, while others show small improvements or small declines depending on the patient, the dose, and the form of treatment. This article goes through these findings step by step so readers can understand the bigger picture.
Finally, this article helps readers understand how experts approach heart safety during TRT. Doctors do not rely on a single cholesterol number to judge risk. Instead, they look at patterns across multiple lab tests, lifestyle factors, and personal health history. They also consider the benefits of treating low testosterone and weigh them against any potential changes in cholesterol or heart function.
By the end of this article, readers will have a clear and detailed understanding of how TRT and cholesterol are connected, what the research shows, and how to discuss heart health with a healthcare provider. The goal is to give people confidence in making informed decisions about their long-term health and well-being.
What Is TRT and Why Does Testosterone Impact Cholesterol?
Testosterone Replacement Therapy, or TRT, is a medical treatment used to raise testosterone levels in people who have low levels due to aging, medical conditions, or injury. Testosterone is a major hormone that affects many parts of the body. Because of this, changing testosterone levels can also change the way the body handles cholesterol, fats, and overall heart health. To understand how TRT and cholesterol are linked, it helps to look at what testosterone does, how it is processed in the body, and how different TRT methods work.
What Testosterone Does in the Body
Testosterone is not just a “sex hormone.” It plays a role in several important systems:
- Metabolism: Testosterone helps regulate how the body uses and stores fat.
- Muscle and bone: It increases muscle mass and helps maintain strong bones.
- Blood production: It signals the body to make more red blood cells.
- Energy and mood: It supports healthy energy levels, motivation, and mood stability.
Because testosterone interacts with many systems, changing its level can influence cholesterol, blood pressure, inflammation, and weight. All of these factors affect heart health.
How Testosterone Affects Cholesterol and Fat Metabolism
Cholesterol is a type of fat that the body needs to make hormones and support cell function. But too much of certain types of cholesterol can raise the risk of heart disease.
Testosterone interacts with cholesterol in several ways:
Testosterone affects how the liver processes fats.
The liver controls cholesterol levels by creating, breaking down, and removing fats from the bloodstream. Testosterone influences how active the liver is in these processes. When testosterone levels change—whether they increase with TRT or decrease due to aging—the liver may handle fats differently. This can lead to increases or decreases in LDL, HDL, or triglycerides.
Testosterone affects body fat distribution.
Lower testosterone levels often lead to more body fat, especially around the abdomen. Abdominal fat is linked to higher LDL, lower HDL, insulin resistance, and higher overall cardiovascular risk. Restoring testosterone to a healthy level may reduce fat in these areas, which can improve metabolic health and indirectly affect cholesterol.
Testosterone affects muscle mass and insulin sensitivity.
More muscle improves how the body handles sugar and fats. Better insulin sensitivity is linked with healthier cholesterol levels. TRT often increases muscle, which may help lower triglycerides and improve metabolic function.
Why Low Testosterone Can Lead to Cholesterol Problems
Before understanding how TRT changes cholesterol, it helps to know what happens when testosterone is low.
People with low testosterone often have:
- Higher body fat
- Lower muscle mass
- Higher insulin resistance
- Higher inflammation
- Higher triglycerides
- Lower HDL (“good” cholesterol)
This means that some cholesterol problems seen during TRT are actually influenced by the pre-existing metabolic state caused by low testosterone itself. In other words, low testosterone can already place the body in a cholesterol-unfriendly state.
Different Forms of TRT and How They Affect the Body
TRT is not a single treatment. There are several ways to deliver testosterone:
Injections
Injected testosterone gives the body a large dose that slowly wears off. Because levels rise and fall more sharply, injections may create bigger swings in cholesterol and red blood cell counts. Some studies show injections can lower HDL more than other methods, especially at high doses.
Gels and creams
These are applied to the skin each day. They provide a steady, stable dose with fewer highs and lows. Because hormone levels stay more even, gels tend to have milder effects on cholesterol. Many doctors prefer this option for patients who have cardiovascular risk factors.
Pellets
Pellets are placed under the skin and release testosterone over several months. They offer stable long-term levels. Some research shows pellets have moderate effects on cholesterol, somewhere between injections and gels.
Patches
Patches provide a controlled release like gels, but some users stop them due to skin irritation. Their effects on cholesterol are generally mild.
Therapeutic TRT vs. Supraphysiologic Doses
It is important to separate medical TRT from the use of anabolic steroids or high-dose testosterone for bodybuilding. Medical TRT aims to bring testosterone into the normal, healthy range, not above it.
- Therapeutic TRT: Usually causes mild or moderate shifts in cholesterol.
- Anabolic steroid abuse: Can sharply lower HDL and increase LDL, raising cardiovascular risk.
This difference is key when reading about testosterone and cholesterol. Much of the severe risk seen in the media comes from non-medical use of high doses.
TRT affects cholesterol because testosterone plays a major role in fat metabolism, liver function, body composition, and insulin sensitivity. Different TRT methods deliver testosterone in different ways, which can change how strongly they affect cholesterol levels. Understanding these basic mechanisms helps explain why some people see changes in their cholesterol while on TRT, and why medical supervision is important for heart health.
How Does TRT Affect Cholesterol Levels Overall?
Testosterone Replacement Therapy (TRT) can affect cholesterol in several ways, and these effects vary depending on dosage, delivery method, age, and a person's overall health. This section explains what current research shows about how TRT changes LDL, HDL, and triglycerides. It also explains why medical TRT behaves differently than anabolic steroid abuse. The goal is to give a clear, simple, and science-based picture of what happens to cholesterol when someone begins testosterone therapy.
TRT and LDL (“Bad” Cholesterol)
Low-density lipoprotein (LDL) is often called “bad cholesterol” because higher levels can raise the risk of plaque build-up in the arteries. Research shows that TRT usually has a mixed effect on LDL levels. What happens depends on the person and the type of TRT used.
Some studies show little to no change in LDL levels when testosterone is used in normal, medically supervised doses. This is especially true in men who start TRT because of clinically low testosterone. For these men, their cholesterol may already be abnormal due to low hormone levels, extra weight, or metabolic problems. When TRT helps those issues, LDL levels may stay the same or even drop slightly.
Other studies, especially those involving higher doses or fast-acting injection peaks, show a small rise in LDL. This rise is usually mild but still important to track. Peaks of testosterone in the blood can affect how the liver processes fats, which may lead to these changes.
Overall, TRT does not usually cause a large increase in LDL, but it can change LDL enough that regular testing is important.
TRT and HDL (“Good” Cholesterol”)
High-density lipoprotein (HDL) helps clear LDL from the bloodstream. Higher HDL levels generally support better heart health.
Among all cholesterol measures, TRT most consistently affects HDL. Many clinical trials show a small drop in HDL, usually between 5–10%. This change does not happen in everyone, but it is common enough that doctors watch HDL closely in TRT users.
Why does the drop happen? Testosterone influences liver enzymes that help regulate fat metabolism. When testosterone levels increase, these enzymes change how they process fats, which can lower HDL levels in some people.
The drop in HDL is usually not large enough to change heart-health risk by itself, especially when men are on well-managed doses. Still, it is a real effect worth watching.
TRT and Triglycerides
Triglycerides are a type of fat carried in the blood. High levels can raise the risk of heart disease and pancreatitis. Research on testosterone shows a more positive trend here: TRT often lowers triglycerides, especially in men who start with low testosterone and metabolic problems such as obesity, insulin resistance, or type 2 diabetes.
Testosterone can improve the way the body handles sugar and fat. When insulin sensitivity improves, triglycerides often go down. Some men will see moderate improvement in their levels after a few months of therapy. Others see little change. But overall, TRT does not usually raise triglycerides, and may help reduce them.
What Clinical Trials Show Overall
Most clinical trials on TRT report the following pattern:
- HDL: mild decrease
- LDL: slight increase, slight decrease, or no change depending on dose and delivery
- Triglycerides: often decrease, especially in men with metabolic issues
- Total cholesterol: usually stays about the same or shifts only slightly
These effects are usually small to moderate, not dramatic. TRT does not behave like anabolic steroids, which are taken at much higher doses and can cause major drops in HDL and significant rises in LDL.
Clinical trials also show that men with obesity, diabetes, or low baseline testosterone may experience improved cholesterol numbers after TRT because their overall metabolic health improves.
Medical TRT vs. Anabolic Steroid Abuse
It is important to separate supervised TRT from anabolic steroid misuse. Steroid abuse uses doses far above medical levels and often includes synthetic hormones that do not act like natural testosterone in the body.
Steroid abuse can cause:
- Very low HDL
- Large spikes in LDL
- Higher blood pressure
- Higher risk of blood clots
These effects are not typical for medically prescribed testosterone.
TRT can change cholesterol, but usually in mild and predictable ways. The most common pattern is a small drop in HDL, often balanced by stable triglycerides and only limited changes in LDL. These effects vary between individuals, which is why monitoring is important.
Does TRT Lower HDL (Good Cholesterol)?
Testosterone Replacement Therapy (TRT) can affect HDL cholesterol, also known as “good cholesterol.” HDL is important because it helps remove excess cholesterol from the bloodstream and carries it back to the liver, where it can be broken down and removed from the body. Higher HDL levels are generally linked to better heart health. Because of this, many people worry when they hear that TRT may lower HDL. This section explains what the research shows, why these changes may happen, and why the effects vary from person to person.
What Research Shows About TRT and HDL Levels
Several clinical studies have looked at how TRT affects HDL levels in adults with low testosterone. Many of these studies show a small drop in HDL in some people who begin testosterone therapy. The decrease is usually mild—often just a few points. For example, someone with an HDL of 55 mg/dL might see it drop to around 50 mg/dL. This amount of change is usually not large enough to put a person at high risk by itself.
However, other studies show very little change or no change at all. A few even show a small increase in HDL, especially in people whose HDL was low to start with due to obesity or poor metabolic health. Because of these mixed results, researchers believe the effect depends on several factors, including how TRT is given, the dose used, a person’s age, body weight, and other health conditions.
It’s important to note that the decrease in HDL seen with TRT is much smaller than the decrease seen with anabolic steroid abuse. High-dose steroids used without medical supervision can cause a strong drop in HDL and a sharp rise in LDL. Medical TRT is different—it uses doses meant to restore normal hormone levels, not raise them beyond the healthy range.
Why HDL May Decrease With TRT
There are several reasons why TRT can lower HDL in some people.
Testosterone Influences Liver Function
The liver controls how the body handles fats and cholesterol. Testosterone can increase the activity of certain liver enzymes that break down HDL particles. This can cause HDL levels to drop slightly, even though the body is functioning normally. For most people, this effect is small.
Testosterone Can Change Fat Distribution
Men with low testosterone often have extra fat, especially belly fat. When TRT helps reduce this fat, it also changes how the body moves and stores cholesterol. In some cases, changes in fat metabolism can cause HDL to dip as the body adjusts to a healthier hormone level.
TRT May Increase Metabolic Rate
Higher testosterone levels increase the body’s energy use and may change how the body processes fats and sugars. These changes can affect HDL because HDL plays a key role in moving fats through the bloodstream.
Individual Health Conditions Play a Role
People with obesity, diabetes, high triglycerides, or heavy alcohol use may see different HDL changes compared to someone without these conditions. In some cases, improving these conditions with TRT and lifestyle changes can help HDL levels rise over time, even if they dip at first.
How Clinically Important Are These HDL Changes?
For most people, the small drop in HDL linked with TRT is not considered dangerous on its own. Doctors look at the entire cholesterol panel, not just HDL. They also look at other risk factors like:
- LDL levels
- Triglycerides
- Blood pressure
- Blood sugar
- Body weight
- Smoking history
- Family history of heart disease
If HDL drops only slightly but other markers improve, the overall effect on heart health may still be positive. For example, if someone loses weight, improves insulin sensitivity, and lowers triglycerides while on TRT, the general direction of their heart health might improve even if HDL goes down a little.
Do Different TRT Methods Affect HDL Differently?
Yes. The type of TRT used can influence HDL changes.
Injectable Testosterone
Injections, especially higher or fluctuating doses, are the most likely to lower HDL. This is because injections can cause short-term spikes in testosterone levels.
Transdermal Gels and Creams
These forms usually have a smaller effect on HDL. They provide a more stable level of testosterone without large peaks.
Pellets
Pellets release testosterone slowly and steadily, and studies show they tend to cause little to no change in HDL for most users.
Because each person responds differently, doctors often choose the form based on both symptoms and lab results.
TRT may lower HDL slightly in some people, but the change is usually small and not dangerous by itself. The effect depends on dose, delivery method, liver metabolism, body weight, and other health conditions. Most importantly, TRT should always be monitored by a healthcare professional. Regular cholesterol testing helps ensure safe treatment and provides a clear picture of how TRT is affecting overall heart health.
Does TRT Raise LDL or Increase Risk of Plaque Build-Up?
One of the most common questions people ask about Testosterone Replacement Therapy (TRT) is whether it raises LDL cholesterol or increases plaque build-up inside the arteries. LDL is often called “bad cholesterol” because high levels can contribute to atherosclerosis, a disease where fatty deposits harden inside blood vessels. Over time, this can raise the risk of heart attack and stroke. Because TRT changes hormone levels throughout the body, it is natural to wonder if it also affects LDL, artery health, and long-term heart risks.
This section explains what current studies show about TRT and LDL, how testosterone may influence plaque inside the arteries, and what factors—such as dose or method of treatment—can change a person’s level of risk.
TRT’s Effect on LDL (Bad Cholesterol)
Research on TRT and LDL has shown mixed results, but several trends appear across many studies:
Small LDL Increases Are Possible in Some Users
Some clinical trials show a small rise in LDL levels in men starting TRT, especially during the first few months. These increases are usually mild and do not push LDL levels into a risky range for most men. However, the change can be more noticeable in men who already have high cholesterol before starting treatment.
Many Studies Show No Significant Change
Other studies find that TRT does not significantly alter LDL levels. In these cases, LDL remains stable or only changes within a normal range. This is more common when TRT is carefully dosed, monitored, and used to treat medical low testosterone—not when taken at high, non-medical doses.
TRT Is Different From Anabolic Steroid Abuse
It is important to separate medically supervised TRT from illegal or abusive use of anabolic steroids. Steroid abuse often leads to large LDL increases and severe drops in HDL. This pattern is not seen in standard TRT dosing. Most concerns about big cholesterol changes come from studies of steroid misuse, not TRT.
Understanding Oxidized LDL and Why It Matters
LDL levels are only one part of the heart health picture. A more harmful type of LDL is called oxidized LDL, which is more likely to stick to artery walls and form plaque. Some research suggests that hormones can influence the oxidation process, but studies on TRT show mixed results:
- Some evidence suggests TRT may even reduce inflammation, which could lower oxidized LDL levels.
- Other studies show no change in oxidized LDL during treatment.
- There is little evidence showing a strong increase in oxidized LDL due to TRT itself.
At this time, most researchers agree that if changes occur, they tend to be mild and heavily influenced by lifestyle, genetics, and underlying health rather than TRT alone.
What Imaging Studies Show About Plaque Build-Up
Doctors use medical imaging to look for plaque inside arteries. Two common tests include:
- Carotid Intima-Media Thickness (CIMT)
- Coronary CT scans
These tests show how thick or hardened artery walls are. Studies using these tools have found:
Some Short-Term Studies Suggest Small Increases in Plaque Thickness
A few trials have reported very small increases in CIMT in men on TRT. These changes were tiny and occurred over long periods, such as one to three years. It’s not clear if testosterone caused the changes, since aging and other health issues can also thicken artery walls over time.
Other Studies Show No Plaque Progression
Several long-term studies show no increase in plaque build-up and no rise in heart attacks or strokes among men on medically supervised TRT. Some even show improved metabolic health, which may protect the heart over the long term.
Dose Matters
Higher-than-normal testosterone levels, especially from overuse or stacking different hormones, have been linked to worse cardiovascular outcomes. Therapeutic doses used to treat true low testosterone do not show these same risks.
How Dose, Formulation, and Hematocrit Influence Risk
Not all TRT methods affect the body the same way. Risk can depend on:
TRT Delivery Method
- Injections may cause quick spikes in testosterone that could stress the cardiovascular system if doses are too large.
- Gels and creams provide a steady, smoother hormone level, which may have a lower impact on cholesterol changes.
- Pellets offer long-lasting hormone levels but can raise testosterone too high if not managed carefully.
Hematocrit Levels
Testosterone can increase hematocrit (the percentage of red blood cells in blood). High hematocrit thickens the blood, which may increase clotting risk. This is not directly related to cholesterol but is important for overall cardiovascular safety.
Individual Health Differences
Men with metabolic syndrome, diabetes, obesity, or a family history of heart disease may respond differently to TRT. In these cases, cholesterol and plaque risk must be monitored more closely.
Current research shows that TRT may cause small LDL increases in some men, but many users see no change at all. TRT does not consistently raise oxidized LDL or cause plaque build-up. Imaging studies show mixed findings, but most research suggests that medically supervised TRT, given in proper doses, does not significantly increase cardiovascular risk. The method of administration, dose control, and monitoring hematocrit levels all play an important role in maintaining heart health during TRT.
What’s the Relationship Between TRT, Triglycerides, and Metabolic Health?
Testosterone plays an important role in how the body handles fats, sugars, and energy. Because of this, Testosterone Replacement Therapy (TRT) can influence triglycerides and overall metabolic health in several ways. Some changes are direct effects of testosterone itself, while others happen because TRT improves or alters other conditions, such as obesity, insulin resistance, or fatigue. Understanding these connections helps patients make informed decisions and work with their medical provider to stay healthy.
How Testosterone Influences Fat Metabolism
Testosterone helps regulate how the body stores and burns fat. Men with low testosterone often gain body fat, especially around the abdomen. This type of fat, called visceral fat, sits deep around organs and plays a major role in raising triglycerides and causing metabolic problems.
When testosterone levels are restored with TRT:
- Fat cells may shrink, especially in the abdominal area
- The body becomes better at using fat for energy
- Lean muscle mass increases, which boosts metabolism
These changes can indirectly improve triglyceride levels. However, not every person will respond the same way, and the degree of improvement often depends on lifestyle habits such as diet and exercise.
How TRT Affects Triglyceride Levels
Triglycerides are a type of fat found in the blood. High levels can raise the risk of heart disease and pancreatitis. Research shows mixed results on how TRT affects triglycerides:
- Many studies show a small drop in triglycerides during TRT
- Other studies report no significant change
- A few studies show increases in triglycerides, but these are less common and usually linked to higher doses or certain delivery methods
Why the differences? Several factors influence how each person’s triglycerides respond to TRT:
Baseline Testosterone Levels
Men with very low testosterone often have higher triglycerides due to insulin resistance and excess body fat. When TRT raises testosterone to normal levels, triglycerides may fall as metabolism improves.
TRT Dose and Method
Different TRT forms release testosterone at different rates:
- Injections create higher peaks and lower valleys
- Gels and patches give more steady levels
- Pellets release testosterone slowly over several months
Because lipid metabolism is sensitive to hormone changes, these patterns can influence triglycerides. More stable testosterone levels may lead to more stable triglyceride levels.
Weight Changes
Many men gain more lean muscle and lose fat on TRT. Fat loss alone can reduce triglycerides. If a patient does not change diet or activity levels, or if calorie intake increases, triglycerides may not improve.
Other Medical Conditions
Patients with diabetes, metabolic syndrome, or thyroid problems may notice more dramatic changes—positive or negative—when starting TRT.
The Role of Insulin Sensitivity in Triglyceride Changes
Insulin is a hormone that helps move sugar into cells. When a person becomes “insulin resistant,” the body must produce more insulin to handle the same amount of sugar. Insulin resistance often leads to:
- Higher triglycerides
- Higher blood sugar
- More abdominal fat
- Fatty liver disease
Low testosterone is strongly linked to insulin resistance. When TRT raises testosterone to healthy levels, several improvements may occur:
- Insulin sensitivity may improve
- Blood sugar may stabilize
- The liver may process fats better
- Triglycerides may decrease
However, these improvements are not guaranteed. The effect is strongest in men whose low testosterone was clearly contributing to insulin resistance.
How Obesity and Metabolic Syndrome Affect TRT's Impact on Triglycerides
Metabolic syndrome is a group of conditions that occur together and increase the risk for heart disease. These include:
- High triglycerides
- Low HDL
- High blood pressure
- High fasting blood sugar
- Large waistline
Men with metabolic syndrome often have low testosterone. In these cases, TRT can sometimes lead to:
- Lower triglycerides
- Mild weight loss
- Improved blood sugar control
But TRT alone cannot fully fix metabolic syndrome. Lifestyle changes are still important.
Why Metabolic Improvements Can Offset Lipid Changes
Some men may see small changes in LDL or HDL during TRT, but these changes may not increase their overall risk because TRT can also improve:
- Body composition
- Blood sugar control
- Energy levels and physical activity
- Inflammation markers
In many cases, the benefits of these improvements outweigh mild shifts in cholesterol numbers.
Does TRT Increase the Risk of Heart Attack or Stroke?
Testosterone Replacement Therapy (TRT) is often prescribed to help men with low testosterone feel better, gain energy, improve mood, and restore normal sexual function. But one of the biggest concerns patients have is whether TRT raises the risk of heart attack or stroke. This question has been studied for years, and the results have sometimes been confusing. Some early research suggested a possible danger, while later studies found little or no increased risk when TRT is used properly. Understanding the evidence can help patients make informed decisions.
Below is a clear explanation of what doctors and researchers know today.
Short-Term vs. Long-Term Cardiovascular Risk
One of the reasons TRT research has mixed results is that studies often look at very different time frames.
Short-Term Risk
Some studies found a small increase in cardiovascular events, such as heart attacks or strokes, during the first 3 to 6 months after starting TRT. This effect is most often seen in:
- Older men
- Men with severe heart disease
- Men starting at very low testosterone levels
- Men receiving very high doses
Researchers believe this early risk may be linked to sudden changes in red blood cell counts, blood thickness, or fluid balance during the first few months of therapy.
Long-Term Risk
Long-term studies—those lasting one to three years or longer—show a different pattern. Many report:
- No increase in heart attacks or strokes
- No rise in cardiovascular deaths
- In some cases, improved heart health markers, such as lower fat mass and better insulin sensitivity
This difference suggests that early monitoring is very important but long-term danger is not clearly supported when TRT is managed carefully.
What Large Studies and Meta-Analyses Show
Over the past decade, many researchers have combined results from multiple studies to get clearer answers. These combined studies are called meta-analyses.
Most recent meta-analyses show that:
- TRT does not significantly raise the risk of heart attack or stroke in men with low testosterone.
- Cardiovascular event rates are similar between men taking TRT and men taking a placebo.
- TRT may improve some risk factors, such as waist size, muscle mass, blood sugar control, and inflammation markers.
However, results vary based on study design, patient age, and overall health. This is why doctors look at individual risk rather than assuming the same effect for all patients.
How Age, Heart History, and Other Conditions Affect Risk
TRT is not equally safe for everyone. Several factors can increase or decrease cardiovascular risk.
Age
Older men, especially those over 65, may have a higher chance of complications in the first few months of therapy. Their blood vessels may already be stiff or narrowed, making them more sensitive to changes in blood viscosity and pressure.
Heart Disease
Men with active or recent heart disease need special caution. This group includes those with:
- Recent heart attack
- Unstable angina
- Severe heart failure
- Major heart rhythm disorders
In such cases, TRT may still be possible but usually requires a cardiologist’s guidance.
High Blood Pressure
TRT can slightly raise blood pressure in some men. If blood pressure is already high or poorly controlled, the added increase could raise stroke risk. Regular monitoring helps catch this early.
High Hematocrit or Thickened Blood
Testosterone can cause the body to make more red blood cells. If hematocrit rises too high, blood becomes thicker and flows less easily. This can increase the risk of clots, which could trigger a heart attack or stroke. This risk is highest with injectable testosterone.
Doctors monitor hematocrit and adjust the dose or pause treatment when needed.
Diabetes or Metabolic Syndrome
For men with insulin resistance, TRT may actually help improve metabolic health, lower visceral fat, and reduce inflammation. These improvements may offset some cardiovascular risks.
How Monitoring and Dosing Reduce Risk
Doctors reduce cardiovascular risk by following clear safety steps:
Baseline Testing
Before starting TRT, clinicians usually check:
- Full lipid panel
- Hematocrit
- Blood pressure
- Blood sugar or A1C
- Cardiovascular history
- Possibly a coronary artery calcium (CAC) scan for older men
Regular Follow-Up
Follow-up visits at 3 months, 6 months, and then every 6–12 months allow doctors to:
- Adjust the dose
- Check for early blood pressure changes
- Monitor hematocrit
- Review cholesterol levels
- Catch side effects early
Tailored Treatment
Different TRT methods can affect heart risk differently.
- Injections may raise hematocrit more.
- Gels or creams usually have a gentler effect on cholesterol and blood thickness.
- Pellets provide very stable testosterone levels.
Doctors choose the method that best matches each patient’s risk profile.
What the Evidence Suggests Overall
Based on current research, TRT does not appear to increase heart attack or stroke risk for most men when used at medically appropriate doses and supervised by a physician. The highest risk occurs in the first months of therapy, especially in older men or those with serious pre-existing heart problems. Careful screening, proper dosing, and routine monitoring greatly reduce these concerns.
How Pre-Existing Cholesterol Problems Change TRT Safety
Testosterone Replacement Therapy (TRT) does not affect every person the same way. Your health before starting treatment plays a major role in how your body responds. This is especially true when it comes to cholesterol and heart health. Some people begin TRT with normal cholesterol levels, while others already have high LDL, low HDL, or issues with triglycerides. These starting conditions can change how safe TRT is, how closely you need to be monitored, and what your healthcare provider may recommend.
This section explains what doctors look for before prescribing TRT, why certain cholesterol problems matter, and what added steps may be needed to stay safe. The goal is to help you understand how your current cholesterol numbers affect your experience with TRT and your long-term heart health.
What Clinicians Evaluate Before Prescribing TRT
Before starting TRT, a medical provider usually reviews your complete heart and metabolic health. This is because testosterone can affect cholesterol, blood pressure, red blood cell levels, and inflammation markers. For people who already have cholesterol problems, this review becomes even more important.
Doctors may check:
- A full lipid panel (LDL, HDL, total cholesterol, triglycerides)
- Blood pressure
- Blood sugar and insulin resistance markers
- Hematocrit and hemoglobin (to see how thick your blood is)
- Your family history of heart disease
- Any past heart issues like stroke, heart attack, or stents
- Body weight and waist size, which relate to metabolic syndrome
If any of these results show a higher-than-normal risk of heart disease, your doctor may talk with you about whether TRT is appropriate, or what steps you need to take before starting.
TRT Considerations for Patients With High LDL
Low-density lipoprotein (LDL) is often called “bad cholesterol” because high levels can contribute to plaque buildup inside arteries. If you already have high LDL, starting TRT may require extra care.
Here’s why:
- Some people experience small increases in LDL during TRT, depending on dose and delivery method.
- If your LDL is already high, even a small increase could raise your long-term risk of heart disease.
- High LDL may also increase the chance of plaque growing inside artery walls over time (atherosclerosis).
In these cases, your provider may:
- Ask you to lower LDL with diet, exercise, or medication before beginning TRT
- Recommend more frequent cholesterol testing
- Suggest keeping testosterone in the lower therapeutic range to avoid unnecessary risk
The goal is not to avoid TRT entirely but to make sure the benefits outweigh the risks.
TRT Considerations for Patients With Low HDL
High-density lipoprotein (HDL) is known as “good cholesterol.” It helps remove excess cholesterol from the bloodstream. Some TRT users notice a small drop in HDL, which can be more concerning if your HDL is already low.
If you start with low HDL, your doctor may:
- Track HDL levels at regular intervals
- Encourage aerobic exercise, which raises HDL
- Suggest nutrition changes, such as adding healthy fats (olive oil, nuts, fish)
- Watch for other heart risk factors that may be harder to balance if HDL falls further
While a mild drop in HDL is not always dangerous, it can matter more for people whose HDL levels are already below normal.
TRT Considerations for Patients With Triglyceride Disorders
High triglycerides can increase the risk of pancreatitis and are strongly linked to insulin resistance and belly fat. Testosterone can influence how your body processes fat and sugar, and these changes may help some people lower triglycerides over time. However, this is not guaranteed.
Patients with high triglycerides may need:
- Closer monitoring of blood sugar and metabolic markers
- A careful look at diet and alcohol intake
- Discussion of medications if triglycerides remain high
For these patients, TRT may help improve metabolic health in some cases, but it must be paired with lifestyle care.
TRT Considerations for Those With a Family History of Heart Disease
If you have close relatives who had early heart attacks or strokes, your long-term risk is already higher. TRT in this situation is not automatically unsafe, but it requires more attention.
Your doctor may recommend:
- Baseline heart imaging, such as coronary artery calcium scoring
- More frequent check-ins after starting TRT
- A conservative dosing plan
Your healthcare provider’s goal is to protect you from avoidable heart stress while still treating low testosterone.
When TRT May Be Contraindicated or Require Extra Monitoring
Although most men can use TRT safely with proper medical oversight, it may be delayed or avoided if you have:
- Uncontrolled high LDL
- Very low HDL
- Severe triglyceride issues
- Active heart disease
- Recent heart attack or stroke
- Very high hematocrit (thickened blood)
If these conditions are present, your clinician may recommend addressing them first. Once controlled, TRT might become safe at a later time.
Monitoring Your Heart Health While on TRT
Monitoring your heart health during Testosterone Replacement Therapy (TRT) is one of the most important parts of safe treatment. Testosterone affects many systems in the body, including blood production, fat metabolism, blood pressure, and cholesterol levels. Because of this, healthcare providers follow certain steps to make sure TRT helps symptoms without increasing heart or cholesterol risks. This section explains, in clear detail, how monitoring works, what tests are needed, how often they should be checked, and when adjustments are necessary.
Baseline Testing Before Starting TRT
Before beginning TRT, a clinician will order a set of tests to understand your starting point. These tests help identify any early problems that could increase heart risk once testosterone levels rise.
Lipid Panel
A lipid panel measures:
- LDL (bad cholesterol)
- HDL (good cholesterol)
- Triglycerides
- Total cholesterol
These numbers show how healthy your cholesterol balance is. If LDL is already high or HDL is low, the provider may recommend lifestyle changes or cholesterol-lowering medication before TRT begins.
Hematocrit and Hemoglobin
Testosterone increases the body’s red blood cell production. This can thicken the blood, raising the risk of clotting, stroke, or heart attack.
Baseline numbers help the provider know your normal range so they can watch for dangerous increases later.
Blood Pressure
High blood pressure strains the heart and arteries. If blood pressure is already high, adding TRT may push it higher. Your provider will check your numbers at the start and track them over time.
Blood Glucose or A1C
These tests check blood sugar levels and insulin resistance. Poor blood sugar control can damage blood vessels and raise heart disease risk. TRT can improve insulin sensitivity, but for some patients it may increase appetite or weight, which can affect blood sugar.
Optional: Coronary Artery Calcium (CAC) Score
A CAC scan shows early plaque buildup in the arteries. It is usually recommended for men over 40 or men with a family history of heart disease. While not required for everyone, it can help guide decisions about TRT if cardiovascular risk is unclear.
How Often to Recheck Cholesterol and Heart Health
Once TRT begins, regular follow-up is essential. Your provider will track how your heart and cholesterol numbers change over time.
Lipid Panel Frequency
- Usually checked 12 weeks after starting TRT
- Then every 6–12 months
If cholesterol changes significantly, testing may be more frequent.
Hematocrit and Hemoglobin Frequency
- At 3 months, 6 months, then every 6–12 months
If hematocrit rises too high (often above 52–54%), the provider may lower the dose, pause TRT, or recommend blood donation to lower levels.
Blood Pressure Monitoring
Blood pressure should be checked:
- At every follow-up appointment
- At home if blood pressure is borderline or high
Home monitoring gives a more accurate picture because readings can vary daily.
Metabolic Monitoring
Your provider may check:
- Blood sugar
- A1C
- Weight
- Waist size
These numbers show how TRT affects body composition and insulin sensitivity.
When Dose Adjustments or Treatment Pauses Are Needed
Sometimes, changes in test results mean TRT must be adjusted. Dose changes are common and do not mean treatment has failed. They are part of safe long-term management.
Reasons for Dose Adjustments
- Hematocrit becomes too high
A reduced dose or switching to a different delivery method (like gel instead of injections) may help. - LDL rises sharply or HDL drops too low
The provider may adjust the dose or add cholesterol management strategies. - Blood pressure increases
Lowering the TRT dose or treating the blood pressure may be necessary. - Symptoms become too strong
If testosterone levels rise above the therapeutic range, side effects such as irritability, acne, or fluid retention may increase cardiovascular stress.
Reasons for Pausing TRT
- Very high hematocrit
- Significant worsening of cholesterol
- New chest pain or heart symptoms
- A new diagnosis of severe heart disease
Pauses are temporary until levels return to a safe range.
Why Monitoring Matters
TRT is safest when the treatment plan includes consistent testing. Most risks linked to testosterone therapy occur when:
- Doses are too high
- Patients do not do follow-up testing
- Blood markers change without being corrected
When monitored properly, TRT can be safe for many patients, including those with mild cholesterol issues.
Lifestyle and Medical Strategies to Support Healthy Cholesterol During TRT
Testosterone Replacement Therapy (TRT) can change the way your body handles fats, cholesterol, blood pressure, and blood sugar. Because of this, your daily habits play a major role in keeping your heart healthy during treatment. Good lifestyle choices can support healthy cholesterol levels, prevent plaque buildup, and reduce cardiovascular risks. They can also improve how your body responds to TRT overall. This section explains the most effective lifestyle and medical strategies to support your heart health in clear, simple detail.
Healthy Eating Patterns That Support Cholesterol Control
Food has a strong impact on cholesterol, especially LDL (often called “bad cholesterol”). The right eating pattern can lower LDL, raise HDL (“good cholesterol”), and reduce inflammation.
Choose heart-focused eating patterns
Several eating styles are backed by strong research for improving cholesterol:
- Mediterranean-style eating
Focuses on fruits, vegetables, whole grains, nuts, beans, olive oil, fish, and lean poultry. This pattern is high in fiber and healthy fats. It has been shown to improve HDL levels and reduce the risk of heart disease. - High-fiber diet
Soluble fiber (found in oats, beans, apples, berries, and barley) binds cholesterol in the gut and helps the body remove it. A daily target of at least 25–30 grams of fiber can lower LDL. - Limiting saturated and trans fats
Foods like fatty red meats, butter, processed foods, fried foods, and bakery items may raise LDL. Choosing lean meats, healthy oils, and whole foods helps keep cholesterol within a healthy range.
Reduce added sugar
High sugar intake raises triglycerides and lowers HDL. Cutting back on sweet drinks, desserts, and refined carbs supports stable blood sugar and healthier cholesterol patterns.
Choose healthier fats
Replace saturated fats with:
- Olive oil
- Avocados
- Nuts (almonds, walnuts, pistachios)
- Fatty fish (salmon, sardines, mackerel)
These fats improve lipid balance and lower inflammation.
Exercise Recommendations for Heart and Cholesterol Health
Physical activity is one of the strongest tools for improving cholesterol levels during TRT. Exercise also helps lower blood pressure and supports a healthy weight.
How exercise affects cholesterol
- Raises HDL (good cholesterol)
- Lowers LDL and triglycerides
- Improves insulin sensitivity
- Reduces body fat, especially belly fat
Types of exercise that work best
- Aerobic exercise
Examples: brisk walking, cycling, swimming, jogging.
Aim for 150 minutes per week of moderate activity or 75 minutes of vigorous activity. - Strength training
TRT already supports muscle growth. Adding strength training twice per week improves fat metabolism and supports heart health. - Daily movement
Small habits like taking the stairs, walking after meals, or stretching during breaks reduce sedentary time and support cholesterol control.
Sleep, Stress, and Daily Habits That Influence Cholesterol
Healthy cholesterol is not only about diet and exercise. Sleep and stress also play a major role in heart health during TRT.
Sleep
Poor sleep raises inflammation, blood pressure, and LDL levels. Aim for:
- 7–9 hours of sleep per night
- A consistent sleep schedule
- A dark, quiet sleeping environment
Sleep apnea is more common in men on TRT. Treating sleep apnea improves cholesterol and overall heart health.
Stress
Chronic stress raises cortisol, which can:
- Increase triglycerides
- Lower HDL
- Raise blood pressure
- Promote weight gain
Stress-reduction practices include:
- Deep breathing exercises
- Light yoga or stretching
- Walking outdoors
- Simple mindfulness routines
- Talk therapy if needed
Medications Often Used With TRT to Support Heart Health
Some people may need medication along with TRT to keep cholesterol and blood pressure in a safe range.
Statins
Statins are the most common cholesterol-lowering medications. They help:
- Lower LDL
- Reduce plaque buildup
- Lower inflammation
Statins can be safely used with TRT when prescribed by a clinician.
Other medications that may be helpful
- Ezetimibe, which lowers cholesterol absorption
- Blood pressure medications, if hypertension develops
- Metformin, for people with insulin resistance or diabetes
- Omega-3 supplements, for high triglycerides (prescription versions are most effective)
Medication needs vary by patient. Your healthcare provider will decide based on lab results and overall risk.
When to Involve a Cardiologist
There are times when a heart specialist should be part of your care plan. This includes:
- A history of heart attack, stroke, or stents
- Very high LDL levels
- A strong family history of early heart disease
- Rapid plaque growth seen on imaging studies
- Chest pain or shortness of breath during TRT
- Elevated blood pressure that does not respond to lifestyle changes
A cardiologist can help guide long-term monitoring and ensure TRT is used as safely as possible.
Key Research Gaps and What Future Studies Are Investigating
Testosterone Replacement Therapy (TRT) has been studied for many years, yet researchers still have many unanswered questions about how it affects cholesterol, heart health, and long-term safety. Even though the medical community has learned a lot, the full picture is not complete. This section explains the main gaps in current research and what future studies hope to uncover. The goal is to help readers understand why results can seem confusing or conflicting and why ongoing studies are important.
Inconsistencies in Study Design
One major problem in TRT research is that studies often use very different methods. This makes it hard to compare results. For example:
Different TRT Forms
Some studies use injections, while others use gels, patches, or pellets. Because each form of TRT releases testosterone into the body in a different way, the effects on cholesterol can vary. A study using injections may show larger changes in HDL or LDL compared to a study using a daily gel. When researchers combine these studies together, the mixed results can make it look like TRT has no clear effect.
Different Doses
Another issue is dosing. Some studies give men the lowest dose needed to bring testosterone into a normal range. Others use higher doses that may raise testosterone to the very top of the normal range. Higher doses can affect cholesterol more strongly. Without consistent dosing rules, the results can be hard to interpret.
Short Study Lengths
Many TRT studies last only a few months. But heart disease takes many years to develop. A study that tracks cholesterol changes for only 12 or 24 weeks may not show important long-term effects. Researchers need studies that last many years to understand whether TRT changes plaque growth, artery stiffness, or overall cardiovascular risk.
Different Patient Populations
Men in TRT studies may have very different health backgrounds. One study may include only older men with low testosterone. Another may include younger men with metabolic syndrome or obesity. Since these groups already have different cholesterol risks, combining their results makes conclusions challenging.
Because of these inconsistencies, scientists cannot yet make absolute statements about TRT’s long-term effects. This is why doctors rely on both research data and individual patient monitoring.
Lack of Long-Term Cardiovascular Outcome Data
Even though many studies measure cholesterol levels, very few measure real-world outcomes like:
- Heart attacks
- Strokes
- Heart failure
- Overall cardiovascular death
- Changes in plaque over time
These are the outcomes that truly matter for heart health. Most existing studies do not follow patients long enough to measure these results. Some studies report slight changes in HDL or LDL, but they do not show whether these changes actually lead to more or fewer heart problems over the course of years.
There is also limited research on how TRT affects specific types of cholesterol, such as oxidized LDL, which plays a bigger role in plaque formation. Without long-term outcomes, doctors must rely on indirect clues instead of direct proof.
Ongoing Trials Examining TRT’s Impact on Atherosclerosis
Atherosclerosis is the process of plaque building up inside the arteries. Several newer studies are now using advanced imaging tools, such as:
- Coronary CT scans
- Ultrasound of the carotid arteries
- Coronary calcium scoring
These tools allow researchers to watch plaque progression over time. Early results have shown mixed outcomes. Some studies show slight increases in plaque thickness in men on TRT, while others show no significant change.
Future trials aim to answer:
- Does TRT speed up plaque growth?
- Does it make plaques more stable or unstable?
- Do cholesterol changes from TRT directly affect plaque buildup?
These questions are important because plaque stability—not just cholesterol numbers—can influence heart attack risk.
Future Directions for Safer, More Personalized TRT
Researchers are also exploring new ways to make TRT safer and more tailored to each patient.
Better Dosing Strategies
Future studies aim to define exact testosterone ranges that provide benefits without increasing cardiovascular risks. This may help doctors choose doses that improve symptoms while protecting heart health.
More Personalized Monitoring
Scientists are studying biomarkers—special blood markers that may predict how a person will respond to TRT. These markers may help identify which patients are at higher risk for cholesterol changes or heart issues.
New TRT Formulations
There is growing interest in longer-acting or more stable TRT forms that may produce fewer fluctuations in testosterone levels. More stable levels may reduce unwanted effects on cholesterol.
Studies in Men With Chronic Conditions
Researchers want to understand how TRT affects men with diabetes, obesity, or metabolic syndrome, since these conditions already increase cholesterol and heart disease risks. These studies may help doctors treat these patients more carefully.
Why These Research Gaps Matter
Until these gaps are filled, doctors must use caution when prescribing TRT. They rely on regular monitoring, patient history, and current evidence. Future long-term studies will help provide clearer answers, guide safer use, and improve care for men who need testosterone therapy.
Conclusion: What We Know Now About TRT and Cholesterol
Testosterone Replacement Therapy (TRT) continues to be one of the most debated treatments in men’s health because it involves two major systems of the body: hormones and the cardiovascular system. After looking closely at current scientific evidence, several clear points emerge about how TRT affects cholesterol and overall heart health. Understanding these points can help patients and clinicians make informed decisions and monitor treatment safely.
First, research shows that TRT does influence cholesterol levels, but the changes are usually modest and vary between individuals. Some people may experience small drops in HDL (“good cholesterol”), while others do not. This decrease is one of the most commonly studied effects of TRT. Although HDL plays an important role in protecting the heart, a mild reduction does not always translate into a higher risk of heart disease, especially when other risk factors are well-controlled. It is important to understand that these changes are typically small in patients who receive medically supervised, appropriate doses of testosterone.
Second, TRT does not consistently raise LDL (“bad cholesterol”) in most studies. Some men show slight increases, others show no change, and a few display improvements. This variation largely occurs because cholesterol levels are affected by many factors beyond TRT, including weight, diet, exercise, insulin sensitivity, and genetics. In some men with low testosterone linked to metabolic syndrome or obesity, TRT may even help improve metabolic health, which can lead to better overall cholesterol patterns. This happens because testosterone plays a key role in how the body uses fat and glucose for energy.
Third, despite common fears, current evidence does not show that medically supervised TRT directly causes plaque buildup in the arteries or a major increase in heart attack or stroke risk for most men. Studies that once raised concern often included older men with serious health problems or used doses far above standard therapeutic levels. More recent, larger, and better-designed studies have been more reassuring, showing no significant rise in cardiovascular events when TRT is used correctly. However, this does not mean TRT is risk-free. Men with a history of heart disease, uncontrolled blood pressure, very high cholesterol, or clotting disorders may face higher risk and need careful evaluation before treatment.
Fourth, individual response to TRT is highly personal. One man may see noticeable improvements in energy, mood, and metabolic health with little to no impact on cholesterol. Another may experience more significant changes in lipids that require closer monitoring. This is why routine testing is essential. Regular checkups allow clinicians to track cholesterol, hematocrit, blood pressure, inflammation markers, and other risk factors. If any value moves into an unsafe range, treatment can be adjusted early. Monitoring makes TRT far safer and helps prevent long-term complications.
Finally, the overall safety of TRT strongly depends on how it is used. The biggest risks appear when testosterone is taken without medical supervision, when doses are too high, or when regular lab work is ignored. These situations can lead to high hematocrit, thickened blood, increased blood pressure, and elevated cardiovascular strain. When TRT is given at the right dose, monitored every few months, and paired with healthy lifestyle habits, the chances of negative heart-related effects drop significantly.
In summary, what we know now is that TRT can affect cholesterol, but the impact is usually small and depends on each person’s unique health profile. TRT does not appear to dramatically raise the risk of heart attack or stroke when used responsibly and with proper follow-up. The key to safe TRT is professional guidance, regular monitoring, and attention to overall cardiovascular health. This includes managing cholesterol, maintaining a healthy weight, exercising, eating well, and treating any other health conditions that may increase risk.
As research continues, we will gain a deeper understanding of how long-term TRT influences heart and vascular health. But at this point, the evidence supports a balanced view: TRT is neither a major heart danger nor a guaranteed benefit. It is a medical therapy that requires thoughtful use, ongoing evaluation, and clear communication between the patient and healthcare provider. With these steps in place, men can use TRT more confidently while protecting their heart health for the long term.
Questions and Answers
TRT may slightly lower HDL (“good”) cholesterol and can sometimes lower or raise LDL (“bad”) cholesterol, depending on the individual and dose.
No. TRT can lower HDL in some individuals, but the change is usually small and not universal.
TRT may influence cholesterol profiles, but the overall cardiovascular risk depends on many factors, including age, lifestyle, and pre-existing conditions.
Yes. Injectable TRT tends to produce larger hormonal swings, which may affect cholesterol more noticeably compared with gels or patches, though effects are still generally modest.
Sometimes. In men with metabolic syndrome or obesity, TRT has been shown to improve triglycerides and occasionally LDL, though results vary.
Yes. Most clinicians recommend checking lipids every 3–6 months when starting TRT, then annually once stable.
TRT doesn’t directly interfere with statins, and many people safely use TRT + statins under medical supervision.
Not necessarily. High cholesterol alone isn’t a contraindication, but doctors often manage lipids first or monitor more closely.
Absolutely. Diet, exercise, weight loss, and reduced alcohol intake remain the primary tools for improving cholesterol, regardless of TRT use.
Normalizing low testosterone can improve metabolism and body composition, which may indirectly help cholesterol, but effects differ widely from person to person.