The Connection Between Testosterone Therapy and High Cholesterol
Introduction
Testosterone therapy, often called TRT, has become a common treatment in recent years. Many men, and some women, are prescribed this therapy when their natural levels of testosterone are too low. Testosterone is a hormone that plays a key role in many functions of the body. It supports muscle growth, bone strength, mood balance, sexual health, and energy levels. As people age, or if they have certain medical conditions, testosterone levels can drop. When this happens, doctors may recommend TRT to help bring hormone levels back to normal.
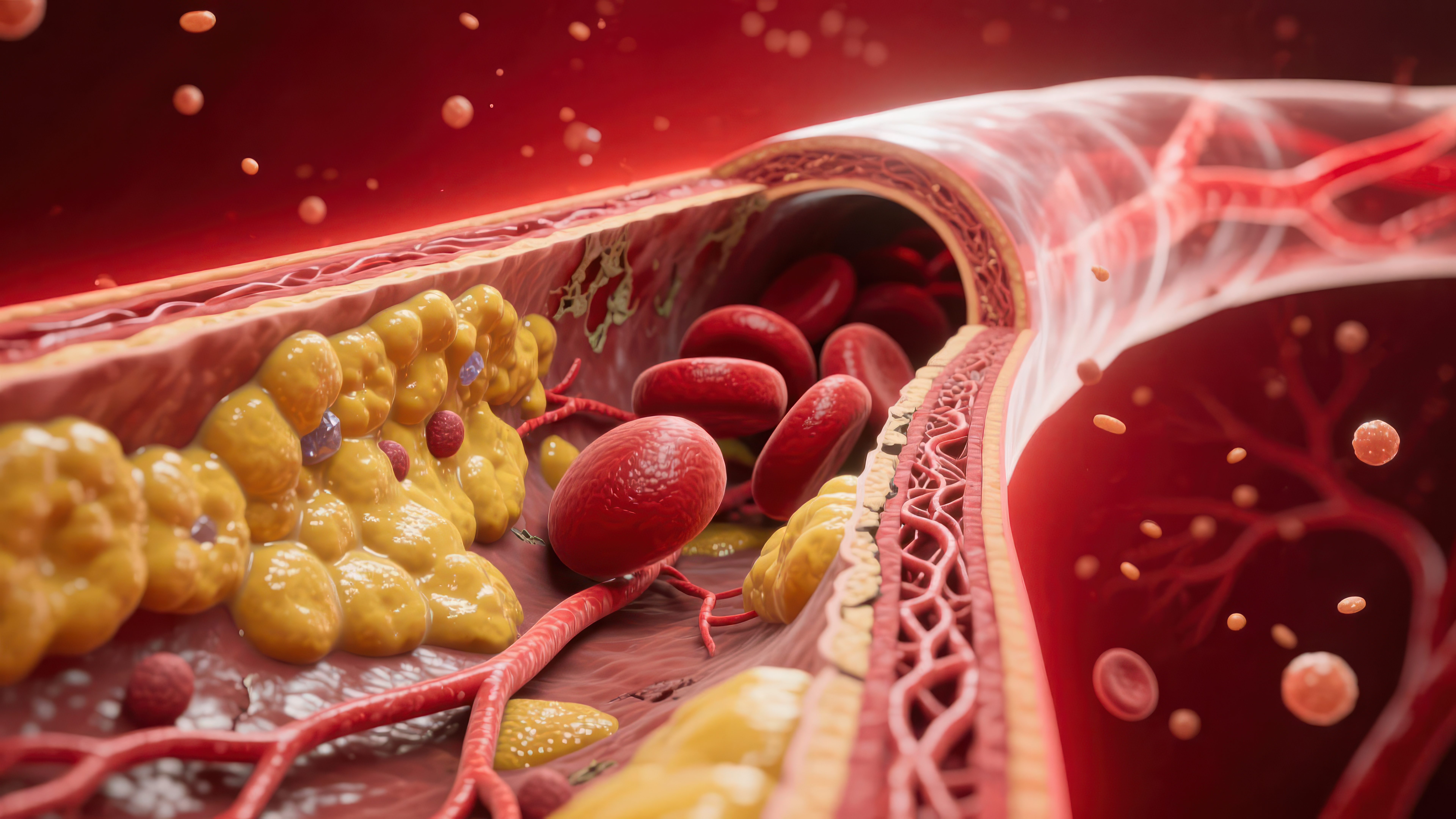
While TRT can improve symptoms of low testosterone, it also raises important questions about safety. One of the biggest concerns is how testosterone therapy may affect cholesterol levels and, in turn, heart health. Cholesterol is a type of fat found in the blood. The body needs some cholesterol to make hormones and keep cells healthy, but too much cholesterol—especially the wrong kind—can build up in blood vessels. This buildup increases the risk of heart disease, stroke, and other cardiovascular problems. Since testosterone is a hormone that interacts with many systems in the body, researchers have long studied whether TRT makes cholesterol better, worse, or has no clear effect at all.
This issue matters because heart disease is one of the leading causes of death worldwide. Millions of people take medication or make lifestyle changes to manage their cholesterol and lower their risk of heart attacks or strokes. At the same time, more men are being treated with TRT than ever before. This overlap means it is very important to understand how testosterone therapy and cholesterol are connected. Doctors and patients need clear information to make safe choices.
The relationship between TRT and cholesterol is not simple. Some studies suggest testosterone therapy can lower certain types of cholesterol, while others show it might reduce the “good” cholesterol that protects the heart. In some cases, TRT seems to have little to no effect at all. These mixed results can be confusing. Part of the challenge is that cholesterol is not just one number. There are different kinds of cholesterol, such as LDL (low-density lipoprotein), HDL (high-density lipoprotein), and triglycerides. Each type plays a different role in health. LDL is often called “bad cholesterol” because high levels can clog arteries. HDL is known as “good cholesterol” because it helps remove LDL from the bloodstream. Triglycerides are another kind of fat that, when high, can also raise heart risks. Testosterone therapy can affect each of these differently, which is why the picture is complex.
Another layer to the issue is that every patient is different. A younger man with otherwise normal health may respond to TRT in one way, while an older man with high cholesterol, diabetes, or obesity may respond in another. Lifestyle factors—such as diet, exercise, smoking, and alcohol use—also play a role. Because of this, doctors usually recommend careful monitoring when someone starts TRT. This often includes checking cholesterol levels and other blood tests on a regular schedule.
The purpose of this article is to answer the most common questions about testosterone therapy and cholesterol. Many people search online to learn whether TRT raises or lowers cholesterol, how it affects heart health, and what risks they should watch for. In this article, we will explain how testosterone works in the body, what current research shows about its effect on cholesterol, and what medical guidelines recommend. We will also discuss factors that can change how TRT interacts with cholesterol, including age, weight, other health conditions, and lifestyle habits. Finally, we will look at what tests and monitoring are needed to keep therapy safe.
By the end of this article, readers should have a clear and balanced understanding of the connection between testosterone therapy and high cholesterol. The goal is not to persuade people for or against TRT, but to provide reliable medical information that is easy to understand. With this knowledge, patients and their doctors can have better conversations, weigh the benefits and risks, and make decisions that fit their health needs.
Testosterone therapy is not just about raising hormone levels—it is about supporting overall health while protecting the heart and blood vessels. Since cholesterol is one of the key markers of heart health, it is vital to study how TRT influences it. This introduction has outlined why the topic matters, why it can be confusing, and why it deserves careful attention. In the following sections, we will explore this subject in detail, starting with what testosterone therapy is, and moving step by step through the science, the risks, and the guidance available today.
What Is Testosterone Therapy (TRT)?
Testosterone therapy, often called TRT, is a medical treatment used to raise testosterone levels in people who have unusually low amounts of this hormone. Testosterone is the main male sex hormone, but it is also found in women in much smaller amounts. It plays a role in sexual health, muscle growth, red blood cell production, bone strength, mood, and overall energy.
When testosterone levels drop too low, people may feel tired, lose muscle mass, gain fat, or have a reduced interest in sex. TRT is one way doctors try to bring hormone levels back to normal. In this section, we will look at what TRT is, the main forms of treatment, why it is used, and how testosterone connects to heart and metabolic health.
What Exactly Is TRT?
TRT means replacing or supplementing testosterone that the body is not making on its own. Doctors prescribe it after checking hormone levels with blood tests. If the results show low testosterone along with symptoms like low energy, poor concentration, or sexual difficulties, TRT may be considered.
It is important to know that TRT is a prescription treatment. It should only be given by a healthcare professional who can monitor hormone levels and overall health. Using testosterone without medical supervision, such as with unregulated supplements or injections from non-medical sources, can be risky.
Different Forms of TRT
TRT can be given in several ways, and each has pros and cons. The main types include:
- Injections – Testosterone is injected into a muscle, often every 1 to 4 weeks. Injections usually cause hormone levels to rise quickly and then slowly drop before the next dose. This up-and-down pattern can sometimes lead to mood swings or changes in energy.
- Gels and Creams – These are applied to the skin daily. The hormone passes through the skin and into the bloodstream. Gels can keep hormone levels more steady but must be used carefully, since the medication can rub off on other people through skin contact.
- Patches – Testosterone patches stick to the skin and release the hormone slowly over time. They are replaced once a day. Patches can cause skin irritation in some people.
- Pellets – Small pellets of testosterone are inserted under the skin by a doctor. They slowly release testosterone for about 3 to 6 months. This method avoids daily or weekly dosing but requires a minor procedure.
- Oral and Buccal Tablets – Some forms of testosterone can be taken by mouth or placed against the gums. However, not all oral forms are safe, since some can affect the liver. Buccal tablets are less common but bypass the liver.
Each method has different effects on convenience, cost, hormone stability, and possible side effects. Doctors choose the best option based on a patient’s health, lifestyle, and preferences.
Why Do People Use TRT?
The main reason for TRT is hypogonadism, a condition where the body cannot make enough testosterone. Hypogonadism can be caused by problems in the testes, the pituitary gland, or the hypothalamus—parts of the body that control hormone production.
Another reason is age-related decline. Testosterone naturally decreases with age, often starting around the late 30s or 40s. While not every man with lower testosterone needs treatment, some may benefit if symptoms are severe and levels are consistently low.
Other medical conditions may also lead to low testosterone, such as obesity, type 2 diabetes, long-term steroid use, chemotherapy, or certain genetic disorders.
Symptoms that may lead to a TRT evaluation include:
- Low energy and fatigue
- Loss of muscle mass and strength
- Increased body fat, especially around the belly
- Low sex drive and erectile dysfunction
- Depressed mood or irritability
- Trouble concentrating
- Reduced bone strength or osteoporosis
If these symptoms are present and confirmed with low hormone levels, TRT may be an option.
Testosterone and Heart/Metabolic Health
Testosterone does more than just affect sexual health. It also plays a role in how the body uses fats and sugars, which is why it may be linked to cholesterol and cardiovascular health.
- Testosterone helps regulate lipid metabolism, which means it affects how cholesterol and fats move through the bloodstream.
- Low testosterone has been linked with higher body fat, insulin resistance, and abnormal cholesterol levels. These are all risk factors for heart disease.
- Some studies show that restoring testosterone to normal levels may improve body composition, lower fat mass, and possibly help balance cholesterol.
However, TRT is not without risks. The exact connection between testosterone therapy, cholesterol levels, and heart health is still being studied. That is why careful monitoring is essential for anyone on TRT.
TRT is a medical treatment designed to restore testosterone levels in people who have low hormone levels and related symptoms. It can be given through injections, gels, patches, pellets, or oral tablets. Doctors use TRT mainly for hypogonadism and sometimes for age-related decline in testosterone. Since testosterone affects more than sexual health—it also influences cholesterol, body fat, and metabolism—understanding its role in heart health is critical.
TRT can improve quality of life for many people, but it requires close medical supervision to balance benefits and risks, especially when it comes to cholesterol and cardiovascular health.
How Does Testosterone Affect Cholesterol Levels?
When people think about testosterone, they often connect it to muscle strength, energy, or sexual health. But testosterone also plays an important role in the body’s metabolism, including the way fats like cholesterol are processed. To understand how testosterone therapy (TRT) may change cholesterol levels, it helps to first look at what cholesterol is, how the body uses it, and then how testosterone interacts with it.
Understanding Cholesterol
Cholesterol is a waxy substance made by the liver. It is also found in certain foods. The body needs cholesterol to build hormones, vitamin D, and healthy cell membranes. Cholesterol is carried in the blood by lipoproteins, which are made up of fats and proteins. The three main types are:
- Low-density lipoprotein (LDL): Often called “bad cholesterol.” High levels of LDL can lead to plaque buildup inside arteries, which increases the risk of heart disease and stroke.
- High-density lipoprotein (HDL): Known as “good cholesterol.” HDL helps carry excess cholesterol back to the liver where it can be removed from the body. Higher HDL levels are protective for heart health.
- Triglycerides: A type of fat that provides energy but, when elevated, can also contribute to cardiovascular problems.
A healthy balance of LDL, HDL, and triglycerides is important for protecting the heart and blood vessels.
Testosterone’s Role in Lipid Metabolism
Testosterone is not just a sex hormone. It affects many systems in the body, including how fats and cholesterol are processed. Research shows that testosterone can influence the way the liver handles cholesterol. For example:
- Testosterone may reduce HDL cholesterol, the protective type. This is a consistent finding in many studies.
- Testosterone’s effect on LDL cholesterol is less clear. Some studies show an increase, others show no change, and some even show a decrease.
- Testosterone can also change triglyceride levels, though the direction of the effect depends on the individual and the type of therapy.
This means that testosterone therapy may shift the overall cholesterol profile, but the exact changes vary from person to person.
Current Research Findings
Studies looking at men receiving TRT show mixed results. Some of the main findings include:
- Decrease in HDL cholesterol:
Many studies agree that testosterone therapy lowers HDL cholesterol. Since HDL is the “good” cholesterol, this change can be concerning. Lower HDL may reduce the body’s ability to remove harmful cholesterol from the bloodstream. - Effects on LDL cholesterol:
The impact on LDL is more complex. In some men, TRT raises LDL slightly, while in others, there is little or no change. The differences may depend on the form of testosterone given (such as injection, gel, or patch), the dose, and the duration of therapy. - Triglycerides:
Some studies suggest TRT may lower triglycerides, especially in men with obesity or metabolic syndrome. Lower triglycerides are generally a positive change. - Overall cardiovascular risk:
Even though TRT can lower HDL, the overall effect on heart disease risk is not fully understood. Some studies show neutral or even beneficial effects of TRT on the heart, while others suggest possible risks.
Why the Results Differ
The reason TRT affects cholesterol differently in people may be due to several factors:
- Age: Older men may respond differently to therapy than younger men.
- Health conditions: Men with obesity, diabetes, or metabolic syndrome may see greater improvements in triglycerides and insulin sensitivity.
- Dosage and method of TRT: Injections, gels, patches, and pellets release testosterone in different ways, leading to different effects on cholesterol.
- Lifestyle: Diet, exercise, and smoking can all change how cholesterol responds to TRT.
Because of these differences, doctors do not assume that TRT will have the same effect on every patient’s cholesterol.
Clinical Meaning of These Changes
The changes in cholesterol from TRT may be small for many men, but they are still important. For example, a small drop in HDL could be meaningful in someone who already has low HDL or high LDL. On the other hand, lowering triglycerides may help reduce risk in men with metabolic problems.
The key point is that TRT can cause changes in cholesterol, but the size and direction of the changes are not the same for everyone. That is why regular blood tests are essential during therapy. Doctors use these tests to check if TRT is helping or harming cholesterol balance and to adjust treatment if needed.
Testosterone therapy affects cholesterol by interacting with the body’s lipid metabolism. The most common finding is a drop in HDL cholesterol, while effects on LDL and triglycerides vary. The changes depend on age, health, lifestyle, and how the testosterone is given. Because cholesterol is closely tied to heart health, men on TRT need regular monitoring to make sure their cholesterol stays in a safe range.
Does TRT Increase the Risk of High Cholesterol?
One of the most common questions men ask before starting testosterone replacement therapy (TRT) is whether it will raise their cholesterol. Cholesterol is a type of fat in the blood that can be both helpful and harmful. Some cholesterol is needed for healthy cells and hormone production, but too much of the wrong kind can lead to clogged arteries, heart disease, or stroke. Because TRT directly affects hormones, and hormones influence cholesterol metabolism, doctors carefully watch how testosterone therapy impacts cholesterol levels.
Understanding Cholesterol and Why It Matters
Cholesterol travels through the bloodstream in particles called lipoproteins. These include:
- Low-density lipoprotein (LDL): Often called “bad cholesterol.” High LDL can cause fatty buildup in arteries, making them narrow and stiff.
- High-density lipoprotein (HDL): Known as “good cholesterol.” HDL helps carry cholesterol away from the arteries and back to the liver to be removed.
- Triglycerides: Another type of fat in the blood. High triglycerides are linked to a higher risk of heart problems.
When people ask about TRT and cholesterol, they usually want to know if it will raise LDL, lower HDL, or increase triglycerides.
Evidence From Clinical Studies
The scientific research on TRT and cholesterol is somewhat mixed, but several patterns appear.
- LDL cholesterol: Some studies show that TRT can slightly raise LDL cholesterol, while others show little to no change. A few reports suggest that men with very low testosterone to begin with may see improvements when levels are restored, but these improvements do not always last long-term.
- HDL cholesterol: More consistently, research shows that TRT may lower HDL levels. This is a concern because HDL protects the heart by clearing cholesterol from arteries. Even a small drop in HDL can affect long-term heart health.
- Triglycerides: In many studies, TRT does not significantly change triglycerides. In some men, especially those who also lose weight while on therapy, triglyceride levels may even improve.
One large review of randomized controlled trials found that TRT caused a modest decrease in HDL and only small changes in LDL and triglycerides. Another long-term observational study noted that men on TRT had lower HDL compared to men not taking it, but their LDL and triglycerides were not much different.
Short-Term vs. Long-Term Effects
It is important to separate what happens in the short-term (first few months) from what happens after years of therapy.
- Short-term therapy (less than 6 months): Cholesterol changes are usually small. HDL may drop slightly, but LDL and triglycerides often remain stable.
- Long-term therapy (over 1 year): Some men continue to have lower HDL over time. LDL may rise in certain patients, especially if they already had borderline or high cholesterol before starting TRT.
This suggests that the longer someone is on testosterone, the more important it becomes to check cholesterol levels regularly.
Why Do These Changes Happen?
The exact reasons are still being studied, but scientists believe testosterone affects the liver, where cholesterol is processed. Testosterone may increase the activity of enzymes that lower HDL and can sometimes raise LDL. It also affects how fats are transported in the blood. For some men, these shifts are minor. For others, especially those with risk factors like obesity, diabetes, or family history of heart disease, the changes may be more noticeable.
Individual Differences Matter
Not every man responds the same way to TRT. The effect on cholesterol can depend on:
- Baseline health: Men who already have high cholesterol or metabolic syndrome may see bigger changes than men with normal cholesterol.
- Type of TRT: Injections, gels, and pellets may have slightly different effects on cholesterol, though the differences are not dramatic.
- Lifestyle factors: Diet, exercise, weight, smoking, and alcohol use all play a role in how cholesterol responds to hormones.
- Age: Older men may have more sensitive cholesterol responses compared to younger men.
Because of these differences, two men on the same TRT plan can have very different cholesterol outcomes.
Does TRT increase the risk of high cholesterol? The answer is not simple. TRT can cause a small drop in HDL and may raise LDL in some men, but the overall effect varies. For some, cholesterol stays stable; for others, it shifts in a less favorable direction. The key is monitoring. Men starting TRT should have a cholesterol test before therapy begins, and then repeat tests every few months during treatment. If levels move in the wrong direction, doctors may adjust the TRT dose, add cholesterol-lowering medication, or suggest stronger lifestyle changes.
Can TRT Improve Cholesterol or Heart Health?
When people hear that testosterone replacement therapy (TRT) may change cholesterol, many wonder if it can actually help improve cholesterol or overall heart health. This is an important question because cholesterol is one of the main risk factors for heart disease, which is still the leading cause of death worldwide. In this section, we will look at how TRT may improve cholesterol, how it affects other parts of heart health, and what the current medical research says.
TRT and Lipid Profiles
Cholesterol is not one single thing—it is a group of fats (lipids) that travel in the blood. The most common types measured are:
- LDL (low-density lipoprotein) – sometimes called “bad cholesterol” because it can build up in the arteries.
- HDL (high-density lipoprotein) – known as “good cholesterol” because it helps clear LDL from the blood.
- Triglycerides – a type of fat that, when high, can also increase the risk of heart disease.
Some studies show that TRT can improve parts of the lipid profile, especially triglycerides. Men with low testosterone often have higher triglyceride levels, and TRT can bring them down to a healthier range. This may lower the risk of developing fatty deposits in the arteries.
The effect on LDL and HDL is less clear. Some men see a small decrease in LDL and total cholesterol. Others show little change. With HDL, the results are mixed as well—some studies report a slight drop in HDL after TRT, while others show no major effect. Doctors continue to watch this closely because even small changes in HDL can matter for long-term heart health.
TRT and Insulin Sensitivity
One way TRT may help the heart is by improving how the body uses insulin. Insulin is the hormone that helps move sugar (glucose) from food into the body’s cells for energy. When the body does not respond well to insulin, it is called insulin resistance. This problem is common in men with low testosterone and is linked to both diabetes and high cholesterol.
Research shows that TRT can improve insulin sensitivity. This means the body can handle blood sugar better, which reduces strain on the pancreas and lowers the risk of type 2 diabetes. Since diabetes often goes hand-in-hand with high cholesterol and heart disease, this improvement may offer indirect protection for the heart.
TRT and Fat Distribution
Another possible benefit of TRT is how it changes body fat and muscle. Low testosterone is linked to higher belly fat, also known as visceral fat. This type of fat builds up deep inside the abdomen around the organs and is especially dangerous for heart health. Visceral fat releases chemicals that increase inflammation, raise triglycerides, and promote plaque buildup in the arteries.
TRT can reduce visceral fat and increase lean muscle mass. A healthier body composition often leads to better cholesterol control, lower blood pressure, and reduced risk of metabolic syndrome (a cluster of conditions including high blood pressure, high blood sugar, and high cholesterol).
Protective vs. Harmful Effects
Even though TRT shows some positive effects, doctors are careful not to call it a “heart treatment.” The results vary depending on the person. Men with very low testosterone may see major improvements, while men with borderline levels may not see much change.
Some studies suggest that TRT could reduce overall heart risk by lowering fat mass, improving blood sugar, and possibly decreasing cholesterol. But other research warns that TRT might increase the risk of blood clots or raise blood pressure in certain cases. Because of this, experts stress the importance of monitoring each patient carefully.
What the Research Tells Us So Far
- Possible benefits: Lower triglycerides, improved insulin sensitivity, reduced belly fat, better muscle mass.
- Unclear effects: LDL and HDL cholesterol changes vary between studies.
- Risks still studied: Potential for blood clotting, changes in blood pressure, or mixed results in men with pre-existing heart disease.
The key takeaway is that TRT may improve some parts of cholesterol and heart health, but it is not a guaranteed “heart protector.” It works best as part of a broader health plan that includes diet, exercise, and medical supervision.
Testosterone therapy can sometimes improve cholesterol and markers of heart health, especially in men who start with very low testosterone and high risk factors. It may lower triglycerides, improve the way the body handles sugar, and reduce belly fat. All of these changes are helpful for the heart. However, because the effects on LDL and HDL are mixed, and because there are still concerns about long-term safety, men should not rely on TRT alone to protect their heart. Regular check-ups, blood tests, and lifestyle changes remain essential.
What Are the Cardiovascular Risks of TRT in Men With High Cholesterol?
Testosterone replacement therapy (TRT) is often prescribed to men who have low testosterone levels. For many men, it helps improve energy, mood, muscle strength, and sexual health. However, when men already have high cholesterol, TRT can raise special concerns. Cholesterol problems increase the chance of developing heart disease, and adding hormone therapy into the mix means doctors must be especially careful. This section explains how TRT and high cholesterol interact, what the risks may be, and why close monitoring is important.
How High Cholesterol Affects the Heart
Cholesterol itself is not “bad.” The body needs it to make hormones, vitamin D, and healthy cell membranes. The problem arises when there is too much low-density lipoprotein (LDL), often called “bad cholesterol.” LDL cholesterol can build up in the arteries, forming plaque. Over time, plaque can harden and narrow the arteries, a process called atherosclerosis. This makes it harder for blood to flow to the heart and brain.
When someone already has high cholesterol, their arteries may already be under strain. They are at a higher risk for conditions such as:
- Heart attack (blocked blood flow to the heart muscle)
- Stroke (blocked blood flow to the brain)
- Peripheral artery disease (poor circulation in the legs or arms)
Because of this background risk, any treatment that might affect cholesterol or blood vessel health—like TRT—deserves extra attention.
How TRT May Change Cholesterol Levels
Research shows mixed results about how testosterone therapy changes cholesterol. Some studies suggest TRT can slightly lower total cholesterol and LDL levels, while others show it may reduce HDL cholesterol (the “good cholesterol” that protects the heart). HDL cholesterol acts like a cleaner, helping carry excess cholesterol away from the arteries. A drop in HDL could weaken this natural protection, especially in men who already struggle with high cholesterol.
These effects may not be dramatic in all men, but when combined with existing cholesterol problems, even small changes could matter over time.
Added Risk of Atherosclerosis
For men with high cholesterol, one of the biggest concerns is whether TRT speeds up atherosclerosis. Testosterone can affect how the body handles fats in the blood, as well as how the blood vessels function. Some research suggests TRT might make arteries stiffer in certain men, while other studies show the opposite—that TRT could improve blood vessel function. Because the evidence is not clear, doctors usually take a cautious approach, especially when high cholesterol is already present.
Risk of Heart Attack or Stroke
There has been debate for years about whether TRT raises the risk of heart attack or stroke. Some early studies suggested possible dangers, but later research, including larger clinical trials, has shown mixed or even reassuring results. The truth may be that the risk depends on individual health factors.
For example, a man with very high cholesterol, obesity, and diabetes may face more risks with TRT than a man with mild cholesterol issues and no other health problems. In short, cholesterol status is one piece of the puzzle, and doctors must look at the whole picture before deciding if TRT is safe.
Why Monitoring Is Critical
Men with high cholesterol who start TRT should expect to undergo regular monitoring. This means:
- Cholesterol checks: LDL, HDL, triglycerides, and total cholesterol should be measured before starting TRT and then checked at regular intervals.
- Heart health tests: Depending on risk level, a doctor may recommend blood pressure checks, blood sugar tests, or even imaging studies to assess artery health.
- Dose adjustments: If cholesterol levels worsen while on TRT, doctors may lower the dose or stop therapy.
This type of monitoring helps catch problems early and allows for treatment adjustments before serious heart issues develop.
The Role of Medications and Lifestyle
It is also important to remember that TRT is not the only factor influencing heart risk. Many men with high cholesterol already take statins or other cholesterol-lowering medications. These drugs can help reduce the risk that TRT might add.
Lifestyle changes—such as eating a heart-healthy diet, exercising regularly, quitting smoking, and keeping alcohol use moderate—play an even bigger role in protecting the heart. When combined with careful monitoring, these steps help balance the possible risks of TRT in men with high cholesterol.
For men with high cholesterol, TRT is not automatically unsafe, but it does carry added cardiovascular risks. The main concerns include possible changes in cholesterol levels, increased risk of artery hardening, and higher chances of heart attack or stroke in certain groups. The best way to lower these risks is through individualized care—working closely with a doctor, tracking cholesterol and heart health, and making lifestyle changes that support long-term cardiovascular protection.
Does TRT Affect HDL Cholesterol (the “Good” Cholesterol)?
When people talk about cholesterol, they often separate it into “bad” cholesterol and “good” cholesterol. HDL, which stands for high-density lipoprotein, is known as the “good” cholesterol. It is considered good because it helps carry extra cholesterol out of the blood and back to the liver, where it can be broken down or removed from the body. Having higher HDL levels usually means a lower risk of heart disease, while lower HDL levels can raise the risk.
Because testosterone replacement therapy (TRT) changes the balance of hormones in the body, researchers and doctors have studied how it affects HDL cholesterol. This is an important question since even small changes in HDL can matter for long-term heart health. Below, we break down what the science shows and what it means for patients.
Why HDL Matters for Heart Protection
HDL cholesterol works like a clean-up system for the blood vessels. It moves cholesterol away from the arteries, which prevents build-up called plaque. Too much plaque in the arteries can lead to a condition called atherosclerosis. Atherosclerosis narrows the arteries and raises the chance of heart attack or stroke.
For this reason, many doctors pay close attention to HDL levels. Even if LDL (“bad” cholesterol) and triglycerides are controlled, a drop in HDL can still make a person’s heart risk higher. So when patients begin TRT, it is natural for doctors to ask: will testosterone lower HDL and reduce this protective effect?
Evidence on TRT and HDL Cholesterol
Research studies on TRT and HDL cholesterol show mixed results. Some studies find that TRT lowers HDL, while others find little to no change. The results often depend on how testosterone is given, the dose, and the health of the person receiving it.
- Injections and higher doses: Some studies report that men who take injectable testosterone, especially in high doses, see a small drop in HDL levels. This effect can appear within a few months of therapy.
- Gels and patches: Men using topical TRT (like gels or patches) often show smaller or no changes in HDL compared to injections.
- Older men vs. younger men: Older men on TRT may have less change in HDL than younger men who receive testosterone for athletic or non-medical reasons.
One consistent pattern is that even when TRT lowers HDL, the decrease is usually modest. For example, HDL might drop by 5–10%. While this is not a huge change, it may still matter for people who already have low HDL or other heart risks.
Why Testosterone May Lower HDL
Scientists believe TRT may reduce HDL for several reasons:
- Hormonal effects – Testosterone may affect enzymes that help regulate how fats and cholesterol move in the body. One enzyme called hepatic lipase can break down HDL, and testosterone may raise the activity of this enzyme.
- Balance with other hormones – When testosterone is increased through TRT, it can change the balance of other hormones, like estrogen. These shifts may influence cholesterol levels.
- Changes in metabolism – Testosterone can change how the liver processes fats, which may affect HDL production and clearance.
These changes don’t affect everyone the same way, which explains why some men see a drop in HDL while others do not.
Clinical Significance of Changes in HDL
A key question is: does a small drop in HDL during TRT matter for overall health? Researchers are still studying this. Some findings suggest that the benefits of TRT, such as improved body composition, lower fat mass, and better insulin sensitivity, may balance out the small drop in HDL.
However, for men with very low HDL before starting TRT, or for men who already have heart disease, even a small reduction could be more concerning. Doctors usually recommend careful monitoring in these cases.
Importantly, a decrease in HDL from TRT does not always mean that a patient’s risk of heart problems will go up. Cardiovascular risk is influenced by many factors, including LDL levels, triglycerides, blood pressure, inflammation, and lifestyle habits.
What Doctors Recommend
Because of the potential for changes in HDL, most guidelines suggest that men on TRT should have their cholesterol levels checked before starting treatment and during therapy. If HDL drops too much, doctors may suggest:
- Adjusting the testosterone dose or method (for example, switching from injections to gel).
- Encouraging lifestyle changes, like regular exercise, a heart-healthy diet, and avoiding smoking, all of which can raise HDL naturally.
- Using medications such as statins if LDL and total cholesterol are also high.
TRT can sometimes lower HDL cholesterol, especially when given in higher doses or through injections. The effect is usually small but may still be important for men with other heart risks. While a drop in HDL is not always dangerous by itself, it highlights the need for regular cholesterol testing and heart health monitoring during TRT.
How Do Other Factors Influence TRT and Cholesterol Relationship?
When doctors look at how testosterone therapy (TRT) affects cholesterol, they know the answer is not the same for every person. Testosterone does not work in isolation. Many other factors, such as age, health conditions, lifestyle, and medications, can change how TRT interacts with cholesterol levels. Understanding these factors is important because they explain why some men may see an improvement in cholesterol while others may see no change or even a negative effect. Let’s explore these one by one.
Age and Baseline Cholesterol Levels
Age plays a big role in both testosterone levels and cholesterol balance. As men get older, natural testosterone levels decline. At the same time, cholesterol levels—especially LDL, the “bad” cholesterol—tend to rise. When an older man starts TRT, his body may respond differently than a younger man’s would.
If a younger man with healthy cholesterol starts TRT, he may not see much change at all. His lipid system is already balanced, so testosterone may have little effect. In contrast, an older man with high cholesterol may notice changes, either better or worse, depending on how his body responds. For example, some studies show TRT can lower total cholesterol slightly in men with abnormal levels, while others suggest it may reduce HDL (the “good” cholesterol) in certain cases.
In short: age and starting cholesterol levels set the stage for how TRT will affect a person’s lipid profile. Doctors often use this information when deciding if TRT is safe for a patient.
Presence of Obesity, Diabetes, or Metabolic Syndrome
Conditions like obesity, diabetes, and metabolic syndrome complicate the picture.
- Obesity: Fat tissue, especially belly fat, affects how hormones are processed in the body. Extra fat can convert testosterone into estrogen through a process called aromatization. This can blunt the effects of TRT and may worsen cholesterol levels if not carefully monitored. Obese men also often have higher triglycerides, which may limit the benefits of TRT on overall lipid health.
- Diabetes: Men with type 2 diabetes often have low testosterone and abnormal cholesterol at the same time. In some cases, TRT can improve insulin sensitivity and reduce blood sugar, which may indirectly help cholesterol. However, results vary. If blood sugar is poorly controlled, the benefits of TRT on cholesterol may be small.
- Metabolic Syndrome: This is a cluster of problems—high blood pressure, high blood sugar, excess abdominal fat, and abnormal cholesterol. In men with this condition, TRT has been shown in some studies to improve waist size and insulin resistance. These changes can help cholesterol levels over time. But again, not every man responds the same way.
These conditions show that TRT is not just about testosterone and cholesterol—it is part of a bigger web of metabolic health.
Lifestyle Factors: Diet, Exercise, Alcohol, and Smoking
Lifestyle choices also play a huge role in cholesterol, and they can change how TRT affects the body.
- Diet: Eating a diet high in saturated fat and processed foods raises LDL cholesterol, no matter what the testosterone level is. If a man starts TRT but keeps an unhealthy diet, he may not see any improvement in cholesterol. On the other hand, combining TRT with a heart-healthy diet (rich in fruits, vegetables, whole grains, and lean proteins) may boost positive effects.
- Exercise: Physical activity is known to raise HDL and lower triglycerides. TRT may increase muscle mass and energy, which could encourage more exercise. This creates a positive cycle: exercise supports good cholesterol, and TRT makes exercise easier.
- Alcohol: Moderate drinking has mixed effects on cholesterol, sometimes raising HDL slightly. Heavy drinking, however, increases triglycerides and damages the liver, which also manages cholesterol. Alcohol abuse may undo any benefits of TRT.
- Smoking: Smoking lowers HDL and increases the risk of plaque buildup in arteries. Even with TRT, smokers may not see improvements in cholesterol and may increase their risk of heart disease.
Lifestyle choices can strengthen or weaken TRT’s effect on cholesterol. This means patients have some control over outcomes.
Interaction With Other Medications Such as Statins
Many men on TRT are also taking medications for cholesterol, blood pressure, or diabetes. These drugs can change how TRT affects the body.
- Statins: These are the most common cholesterol-lowering drugs. Research suggests TRT can be used safely alongside statins. In fact, both therapies may complement each other—statins lower LDL, while TRT can help improve energy, lean muscle, and metabolic function. But close monitoring is needed to be sure the combination does not lead to very low cholesterol or unwanted side effects.
- Blood pressure drugs and diabetes medications: These may not directly affect cholesterol, but they influence heart and metabolic health. Since TRT also affects these systems, doctors often look at the full list of medications before starting therapy.
Interactions remind us that TRT is not used in isolation. It must fit into a broader medical plan.
TRT’s effect on cholesterol is shaped by much more than just testosterone levels. Age, starting cholesterol numbers, obesity, diabetes, and metabolic syndrome all change how the body responds. Lifestyle choices—what a man eats, how much he exercises, and whether he smokes or drinks—can either strengthen or weaken TRT’s effects. Finally, other medications, especially statins, also play a role.
This is why doctors rarely make blanket statements like “TRT lowers cholesterol” or “TRT raises cholesterol.” The reality is more complex. The outcome depends on the whole health picture of the patient. For men considering TRT, this means close monitoring and open conversations with their healthcare provider are essential.
What Blood Tests Are Needed to Monitor TRT and Cholesterol?
When a man starts testosterone replacement therapy (TRT), it is important to track how his body responds. Testosterone can affect many systems in the body, including the heart, liver, and blood. One of the most important areas to watch is cholesterol and other blood fats. Doctors use regular blood tests to keep TRT safe and to make sure it is not causing new health problems.
This section explains the main blood tests used before starting TRT and during treatment. It also covers how often these tests should be done and why they matter.
Blood Tests Before Starting TRT
Before a man begins TRT, doctors want to understand his health baseline. This means checking his hormone levels and his overall risk for heart disease. The most common tests include:
- Total Testosterone Test
- Confirms low testosterone before therapy begins.
- Usually measured in the morning when levels are highest.
- Cholesterol Panel (Lipid Profile)
- Measures total cholesterol, LDL (bad cholesterol), HDL (good cholesterol), and triglycerides.
- Helps show whether a man already has high cholesterol or other risks for heart disease.
- Liver Function Tests (LFTs)
- The liver helps process both cholesterol and hormones.
- These tests make sure the liver is healthy enough to handle TRT.
- Complete Blood Count (CBC)
- Measures red blood cells, white blood cells, and platelets.
- Testosterone can raise red blood cell levels, which increases the risk of blood clots.
- Other Baseline Markers
- Blood sugar (fasting glucose or HbA1c) to check for diabetes or prediabetes.
- Kidney function tests to make sure the kidneys are healthy.
By having these tests before starting, doctors can compare later results to see if TRT is making positive or negative changes.
Ongoing Monitoring During TRT
Once treatment begins, regular blood tests are needed to watch for changes. Most doctors check within 3–6 months after starting, then every 6–12 months after that. If problems are found, testing may be more frequent.
Here are the key tests during TRT:
- Cholesterol Panel (Lipid Profile)
- The most important test for heart health during TRT.
- Measures LDL, HDL, and triglycerides.
- LDL should stay low, HDL should stay in a healthy range, and triglycerides should not rise too much.
- Total and Free Testosterone
- Confirms that TRT is raising testosterone to the right level, not too low or too high.
- Helps doctors adjust the dose if needed.
- Complete Blood Count (CBC)
- Checks for polycythemia, which is when red blood cells become too high.
- If red blood cells get too high, the doctor may lower the TRT dose or suggest blood donation to lower the risk of clots.
- Liver Function Tests
- Important for men using oral or injectable testosterone, since the liver processes hormones.
- High liver enzymes may mean the liver is under stress.
- Blood Sugar and Metabolic Markers
- Some men on TRT see changes in insulin sensitivity.
- Monitoring fasting glucose or HbA1c helps track diabetes risk.
- Other Optional Tests
- PSA (Prostate-Specific Antigen): for men over 40, especially if there is concern about prostate health.
- C-reactive protein (CRP): measures inflammation, which may relate to heart health.
Why Monitoring Cholesterol Is So Important
Cholesterol and other lipids are central to the debate about TRT and heart health. Some studies suggest TRT may lower triglycerides or improve insulin sensitivity. Others show it may reduce HDL cholesterol, which protects against heart disease. Because results vary, regular lipid testing is the best way to stay safe.
If LDL cholesterol goes up while on TRT, the doctor may:
- Recommend lifestyle changes like a healthier diet or more exercise.
- Prescribe medications like statins to lower cholesterol.
- Adjust the testosterone dose or delivery method.
Frequency of Blood Tests
- First 3–6 months after starting TRT: cholesterol panel, testosterone levels, CBC, and liver tests.
- Every 6–12 months after that: repeat the same tests, unless there are concerns that require earlier checks.
- Anytime symptoms appear: such as chest pain, shortness of breath, unusual fatigue, or swelling, doctors may order extra tests right away.
Blood tests are not just routine—they are the foundation of safe TRT. They help catch problems early, before they become serious. For cholesterol, a full lipid panel is the most important. But it should always be combined with tests for liver health, blood cell counts, and hormone levels. With careful monitoring, TRT can be managed in a way that balances the benefits of hormone therapy with protection for the heart and blood vessels.
What Do Guidelines Say About TRT and Cholesterol Management?
When it comes to testosterone replacement therapy (TRT), many men want to know what the official medical guidelines recommend, especially when it comes to cholesterol and heart health. Because TRT can affect blood lipids in different ways, professional medical groups have issued guidance on how doctors should monitor patients and reduce risks. These recommendations help ensure that treatment is both safe and effective.
The Role of Medical Guidelines
Medical guidelines are sets of recommendations created by experts. They are based on large research studies, clinical trials, and years of medical experience. Their purpose is to guide doctors in making safe choices for patients. With TRT, guidelines focus on when therapy should be started, how it should be monitored, and how to manage potential side effects, including high cholesterol.
Major Organizations That Provide Guidance
Several respected organizations have released official recommendations about TRT:
- The Endocrine Society – an international group of hormone specialists.
- The American Urological Association (AUA) – focused on men’s health and testosterone use.
- The American College of Cardiology (ACC) and American Heart Association (AHA) – provide advice on cholesterol and heart disease.
- The FDA (U.S. Food and Drug Administration) – regulates medications, including testosterone products.
Together, these groups form the backbone of safe practice for testosterone therapy and cholesterol monitoring.
Starting TRT: Baseline Testing
All major guidelines agree that before starting TRT, doctors should order blood tests to measure:
- Total cholesterol
- LDL cholesterol (bad cholesterol)
- HDL cholesterol (good cholesterol)
- Triglycerides
- Liver enzymes
- Blood sugar (glucose or HbA1c)
The goal is to understand a man’s baseline health before therapy begins. If a patient already has very high cholesterol or uncontrolled heart disease, guidelines suggest treating those conditions first or carefully weighing risks and benefits before starting TRT.
Ongoing Monitoring Once on TRT
Guidelines stress the importance of continuous monitoring because TRT can change cholesterol levels and affect the heart. Recommended monitoring includes:
- Lipid panel (cholesterol tests) every 3–6 months during the first year.
- Yearly cholesterol checks once stable.
- Liver function tests at similar intervals.
- Heart health evaluation, especially if the patient has other risk factors like obesity, diabetes, or smoking.
If cholesterol worsens while on TRT, guidelines recommend adjusting treatment. This might mean lowering the TRT dose, changing the delivery method (for example, switching from injections to gels), or adding cholesterol-lowering medication such as statins.
Thresholds for Intervention
Professional guidelines also define “thresholds” that trigger medical action:
- LDL cholesterol over 160 mg/dL: most guidelines recommend starting cholesterol-lowering treatment if lifestyle changes do not help.
- HDL cholesterol below 40 mg/dL: considered a red flag, since TRT may sometimes reduce HDL.
- Triglycerides above 200 mg/dL: signals increased risk for heart disease and requires attention.
If any of these changes occur while on TRT, doctors may adjust therapy, recommend lifestyle improvements, or prescribe medication to bring cholesterol under control.
Balancing Benefits and Risks
The AUA and Endocrine Society both emphasize that TRT should only be given to men with confirmed low testosterone levels and symptoms. They caution against using testosterone simply for “anti-aging” or performance enhancement. For men who truly need TRT, the benefits can be significant—improved energy, mood, bone health, and sexual function. But these benefits must always be balanced against the possible risks to cholesterol and heart health.
Cardiovascular Considerations
The ACC and AHA guidelines highlight that men with known heart disease or very high cholesterol should be closely monitored if they start TRT. Doctors may involve a cardiologist in these cases. The reason is that testosterone can influence red blood cell counts, blood pressure, and lipids—all of which can increase cardiovascular risk if not controlled.
Safety Protocols Recommended
Across different organizations, some safety protocols are repeated:
- Confirm diagnosis first – TRT should not be given without at least two morning blood tests showing low testosterone.
- Check cholesterol regularly – because TRT can affect lipid balance.
- Promote healthy lifestyle – diet, exercise, weight control, and smoking cessation are essential.
- Avoid overtreatment – guidelines warn against pushing testosterone levels too high, since this can worsen cardiovascular risks.
The Role of Shared Decision-Making
Guidelines stress that decisions about TRT should involve both doctor and patient. This is called shared decision-making. The doctor explains potential benefits and risks, including cholesterol effects, and the patient helps decide whether to proceed. This process ensures that men fully understand what monitoring and lifestyle changes will be needed.
Can Lifestyle Changes Help Manage Cholesterol While on TRT?
When someone is taking testosterone replacement therapy (TRT), it is important to keep a close eye on heart health and cholesterol levels. TRT can sometimes change the balance between LDL (“bad” cholesterol), HDL (“good” cholesterol), and triglycerides. While doctors may recommend medications like statins if cholesterol gets too high, lifestyle choices play a huge role in controlling cholesterol and reducing the risk of heart disease. In fact, healthy daily habits can often strengthen the positive effects of TRT and lower the risks.
Let’s explore the main lifestyle changes that can help keep cholesterol under control while on testosterone therapy.
Importance of Diet
Diet is one of the strongest tools for managing cholesterol. What you eat directly affects the levels of LDL, HDL, and triglycerides in the blood.
- Limit saturated and trans fats: Saturated fats are found in red meats, butter, cheese, and other animal-based products. Trans fats are often hidden in fried foods, packaged snacks, and baked goods. Both types of fat can raise LDL cholesterol, which contributes to plaque buildup in arteries. Replacing these fats with healthier options is key.
- Choose healthy fats: Unsaturated fats, especially omega-3 fatty acids, are protective for the heart. Foods like salmon, tuna, walnuts, chia seeds, flaxseeds, and olive oil can help lower triglycerides and improve overall cholesterol balance.
- Increase fiber intake: Soluble fiber, found in oats, beans, lentils, apples, and pears, binds to cholesterol in the digestive system and helps remove it from the body. Aiming for 25–30 grams of fiber each day can lower LDL cholesterol.
- Focus on whole foods: Diets that emphasize fruits, vegetables, whole grains, lean proteins, and nuts—like the Mediterranean diet—are linked to better cholesterol levels and lower rates of heart disease.
- Cut down on added sugars: High sugar intake can raise triglycerides and lower HDL cholesterol. Sugary drinks, desserts, and processed foods should be limited.
When combined with TRT, a heart-healthy diet helps reduce cholesterol swings and supports long-term cardiovascular protection.
Exercise and Physical Activity
Regular physical activity is another powerful way to keep cholesterol balanced while on TRT. Exercise helps lower LDL and triglycerides while increasing HDL cholesterol.
- Aerobic exercise: Activities like brisk walking, jogging, cycling, or swimming improve circulation and lower blood lipids. At least 150 minutes of moderate-intensity aerobic exercise each week is recommended.
- Strength training: Lifting weights or using resistance bands at least two days per week helps build lean muscle. This not only boosts metabolism but also improves insulin sensitivity, which can reduce triglycerides.
- Daily movement: Small changes like taking the stairs, walking during breaks, or standing instead of sitting for long hours add up. Consistency is more important than intensity for many people.
TRT may improve energy and muscle mass, which can make exercise feel easier and more rewarding. Using this added strength to stay active can greatly benefit cholesterol control.
Weight Management
Maintaining a healthy weight is directly tied to cholesterol levels. Extra body fat, especially around the waist, is linked to higher LDL cholesterol and triglycerides as well as lower HDL cholesterol.
TRT can sometimes help reduce fat mass and increase lean muscle, but lifestyle choices are still critical. Eating a balanced diet, avoiding overeating, and staying active all help maintain a healthy weight. Even a modest weight loss of 5–10% of body weight can lead to significant improvements in cholesterol and heart health.
Alcohol and Smoking
Both alcohol and smoking play a major role in cholesterol and heart health.
- Alcohol: Moderate alcohol use can sometimes raise HDL cholesterol, but drinking too much raises triglycerides and blood pressure. For men on TRT, heavy alcohol use can also affect liver health and hormone balance. Most experts recommend limiting alcohol to no more than two drinks per day for men, and less if possible.
- Smoking: Cigarette smoking lowers HDL cholesterol and damages blood vessels, making cholesterol buildup worse. Quitting smoking can quickly improve HDL levels and reduce the risk of heart disease.
For men on TRT, avoiding smoking and keeping alcohol in check reduces risks and supports overall treatment goals.
Working With Healthcare Providers
Lifestyle changes are most effective when combined with regular medical care. Doctors often recommend cholesterol tests before starting TRT and then at regular intervals. If cholesterol levels rise, adjusting diet, exercise, or alcohol intake may help. In some cases, a doctor may suggest cholesterol-lowering medication along with TRT.
Being open about lifestyle habits—such as diet choices, smoking, or alcohol use—helps healthcare providers give more personalized advice.
Testosterone therapy and cholesterol are closely connected, but lifestyle choices give patients a strong way to manage their risks. A diet rich in whole foods and healthy fats, regular exercise, healthy weight control, limited alcohol, and avoiding smoking can make a huge difference. These habits not only improve cholesterol but also support better heart health, energy levels, and overall well-being while on TRT.
Conclusion
Testosterone therapy, often called TRT, has become an important treatment for men with low testosterone. Many men use it to improve energy, mood, sexual health, and overall well-being. But like any medical treatment, it comes with both possible benefits and risks. One of the most important health areas to understand is how TRT connects to cholesterol and heart health. Cholesterol is a key factor in cardiovascular disease, which is still the leading cause of death worldwide. Because of this, doctors and patients need to pay close attention to cholesterol changes during TRT.
The research shows that testosterone therapy can affect cholesterol in different ways, and these effects are not the same for everyone. Some studies have found that TRT can raise LDL cholesterol, which is known as “bad cholesterol” because it can build up in arteries and cause heart disease. At the same time, TRT can sometimes lower HDL cholesterol, which is “good cholesterol” because it helps remove harmful fats from the blood. Changes in triglycerides, another type of fat in the blood, have also been reported. These shifts may be small in some men, but more noticeable in others. This shows that testosterone therapy does not have a one-size-fits-all effect.
Other research suggests that TRT may improve some markers of heart and metabolic health. For example, it may help reduce body fat, improve muscle mass, and improve insulin sensitivity, which is the way the body responds to blood sugar. These benefits could indirectly help cholesterol and reduce heart risk in certain men. Still, the results across studies are mixed. Some men may see improvements, while others may not. This makes regular monitoring very important.
One of the most important things to consider is whether a man already has high cholesterol or other heart risk factors before starting TRT. If cholesterol is already high, or if there is a history of heart disease, the risks of TRT may be greater. TRT could potentially make cholesterol worse in these men, raising the chance of heart problems like heart attack or stroke. That does not mean TRT must be avoided in every case, but it does mean doctors need to carefully check blood tests before treatment and keep monitoring during therapy.
Blood tests are the most reliable way to track how TRT is affecting cholesterol and overall health. These tests should include total cholesterol, LDL, HDL, triglycerides, and sometimes additional markers like liver enzymes and blood sugar levels. Doctors usually check these before starting TRT, then several months after treatment begins, and then on a regular schedule after that. If cholesterol levels change in a harmful way, treatment may need to be adjusted. Sometimes the dose or method of TRT is changed, or medications like statins may be added to control cholesterol.
Guidelines from major medical groups, such as the Endocrine Society and the American Urological Association, also highlight the need for careful monitoring. They do not say that TRT must be avoided in all men with high cholesterol, but they do recommend close supervision. The focus is on balance: treating the symptoms of low testosterone while also protecting long-term heart health.
Lifestyle choices are another important part of the picture. Men on TRT can take active steps to reduce cholesterol risk. Eating a healthy diet that is low in saturated fats and rich in fruits, vegetables, lean proteins, and whole grains is very helpful. Exercise, especially a mix of aerobic activity and strength training, can improve both testosterone levels and cholesterol. Maintaining a healthy weight, avoiding smoking, and limiting alcohol also make a big difference. These habits work together with medical treatment to keep the heart and blood vessels healthy.
In the end, the connection between testosterone therapy and cholesterol is complex. TRT is neither entirely harmful nor entirely protective when it comes to cholesterol. Its effects depend on the individual man, his overall health, his starting cholesterol levels, and how closely his treatment is managed. The key takeaway is that men who use TRT should not ignore cholesterol. Regular testing, open communication with healthcare providers, and healthy lifestyle choices all help reduce risks.
Testosterone therapy can bring real improvements in quality of life for men with low testosterone. But it should always be used with careful medical supervision, especially when it comes to cholesterol and heart health. With the right balance of treatment, monitoring, and healthy habits, many men can use TRT safely while keeping their cholesterol under control.
Questions and Answers
Yes. TRT can influence cholesterol levels, sometimes lowering HDL (“good” cholesterol) and occasionally raising LDL (“bad” cholesterol) or triglycerides. The exact effect varies by individual, dose, and delivery method.
HDL cholesterol helps clear excess cholesterol from the bloodstream. If TRT lowers HDL, it may reduce this protective effect, potentially increasing cardiovascular risk.
Yes. In men with low testosterone and metabolic syndrome, TRT may improve lipid profiles, reduce triglycerides, and modestly lower LDL. However, responses differ person to person.
It can. Injectable testosterone may have stronger impacts on lipids compared to gels or patches, though evidence is mixed. Topical forms may cause fewer fluctuations in cholesterol.
Doctors usually recommend a lipid panel before starting TRT, then again 3–6 months after initiation, and at least yearly thereafter. Monitoring helps catch unfavorable changes early.
Yes. Pre-existing high cholesterol combined with TRT-related changes may increase cardiovascular risk. That’s why risk-benefit evaluation and close monitoring are crucial.
Absolutely. Eating a heart-healthy diet, exercising regularly, avoiding smoking, and limiting alcohol can counterbalance negative lipid changes from TRT.
There’s no major drug-drug interaction between TRT and statins. In fact, men on TRT who also have high cholesterol may benefit from statin therapy to reduce cardiovascular risk.
Yes. TRT can increase lean body mass, reduce visceral fat, and improve insulin sensitivity. These metabolic improvements may lead to healthier cholesterol levels in some men.
They should undergo a full cardiovascular risk assessment, discuss options with their doctor, and create a plan for regular cholesterol monitoring and lifestyle modifications.