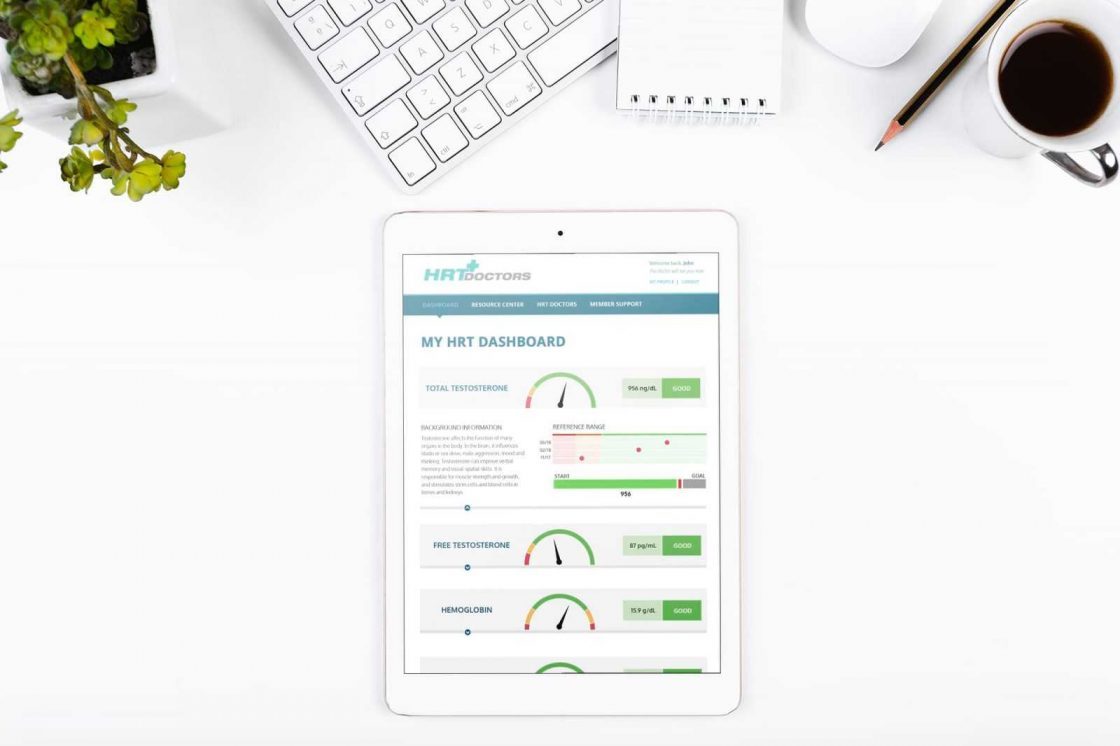
Online Hormone Replacement Therapy – HRT Clinics
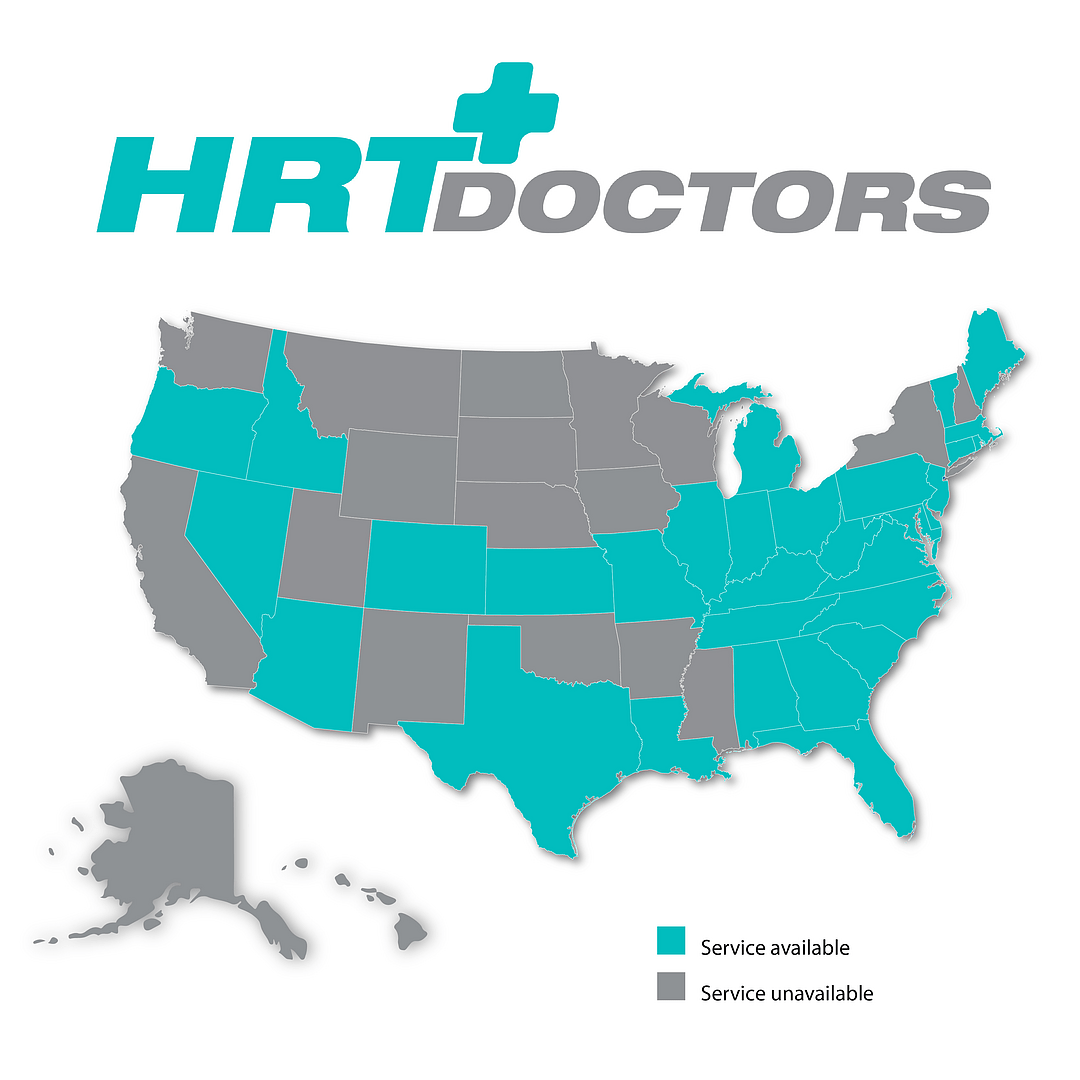
HRT Doctors is a nationwide Telemedical Clinical Practice and an online HRT Clinic, specializing in Hormone Replacement Therapy (HRT) for men and women. If you are considering Hormone therapy, we are an online HRT Clinic that is a convenient and affordable alternative. We are fully licensed and provide service to 38 states nationwide.
At HRT Doctors Group, the leading online HRT clinic, every doctor is an expert in HRT. $89.95 includes a comprehensive hormone blood test at your local Quest Diagnostics and an in-depth consultation with one of our board-certified doctors.

 Lab & Telehealth Medical Review
Lab & Telehealth Medical Review Testosterone injections
Testosterone injections Testosterone Cream
Testosterone Cream Anastrozole Tablets
Anastrozole Tablets Enclomiphene Citrate Capsules
Enclomiphene Citrate Capsules Doctor Follow-up Visits
Doctor Follow-up Visits
Are you ready to improve your health and boost your energy with Hormone Replacement Therapy? Our online services provide a straightforward way to enhance the quality of your life. Let’s take a closer look at how this treatment can help you:
Unpacking hormone therapy
Hormone Replacement Therapy (HRT) is a medical treatment aimed at balancing hormone levels in the body. It’s particularly beneficial for individuals facing issues related to andropause (often referred to as male menopause).
Many people choose HRT through telemedicine with the hope of improving their quality of life. If you’re a man wanting to boost vitality and manage symptoms, HRT might be what you need.
Getting started with HRT is easy and convenient thanks to our telemedicine services.
It’s as easy as 1-2-3
- Blood Test: Upon completing the patient on-boarding forms, our patient care team will send you a Quest Diagnostics lab requisition. You can complete this blood test at any local Quest Diagnostics. Once the results come back, our patient care team will schedule a telemedicine consultation with one of our board-certified Doctors.
- Consultation Assessment: During the consultation, our Doctors will assess your well-being and determine whether hormone replacement therapy is appropriate for you or not. If an underlying condition is found, you will be referred back to your Doctor or a specialist. If it’s determined that you are an appropriate patient for hormone therapy, a specific protocol will be recommended and the script will be conveniently sent to our pharmacy.
- Individualized Strategy: Using your evaluation as a foundation, you’ll receive a tailored program, carefully crafted to align with your unique requirements, symptoms, and goals.
Exploring solutions: Customized medical protocols for patients
HRT for Men: Boosting Vitality
Men experience a similar phase known as andropause, marked by hormonal changes that can affect their mood, energy, and overall life quality. Hormone treatment plans for men aim to rejuvenate their vitality, improve mood, and enhance life quality. This can lead to a revival of self-confidence and overall well-being for men.
BHRT: Bio-Identical Hormone Replacement Therapy
By using hormones that are chemically identical to those your body naturally produces, BHRT aims to restore balance and well-being. BHRT is used to address hormonal imbalances in men, such as those caused by low testosterone levels. This can help alleviate fatigue, decrease in sexual desire, and loss of muscle strength. The therapy can be administered in several forms, including creams, gels, injections, and even pellets inserted under the skin, making it a versatile option for many.
However, despite its benefits and “natural” label, BHRT is not without risks. Potential side effects can include an increased risk of blood clots, stroke, and certain types of cancer. Always consult a healthcare provider for a thorough evaluation and to discuss whether BHRT or any other form of hormone replacement therapy is appropriate for you.
- Protocol Choices: Navigating the Possibilities
- Cream Protocol: Convenient and easily assimilated into your daily routine.
- Endogenous Patches: Patches deliver a static dosage and are thus not an option for the variable dosing methodology.
- Endogenous Creams and Gels: Applied directly to the skin for absorption, offering precise control over the dosage by using a click-dial bottle. Each click dispenses 1ml.
- Pellet therapy: Implanted beneath the skin, these pellets release endocrine factors gradually, providing prolonged relief. Since our practice utilizes telemedicine, our Doctors do not work with pellets.
- Injections: Male protocols are offered in an injection format. However, female protocols are not available as an injection.
Selecting the best treatment option is a highly personal decision. Your medical history, lifestyle, and specific treatment objectives are key factors that will influence your choice. It’s crucial to consult with a board-certified doctor or your personal physician to make an informed decision.
Addressing hormone imbalances can offer significant hope for improvement.
This kind of treatment offers several key benefits



Balancing Act: Evaluating the Risks
Now let’s look at the other side of the coin: treatment isn’t without risks, and it’s important to understand them:
Heart Risks: For some people, especially those with existing heart problems, treatment could increase the chance of heart-related issues. It’s important to carefully consider the benefits and risks.
Blood Clots: In some situations, treatment could raise the risk of developing blood clots, similar to unexpected bumps in the road.
Cancer Questions: There are ongoing debates about whether treatment could be linked to certain cancers, like breast cancer. This calls for a cautious approach.
Our Doctor consultation will address these respective risks and considerations.
When HRT may not be right for you?
Here are some factors that could rule out hormone replacement therapy (HRT) as an option for you:
Active Cancer:
HRT may not be recommended for those with certain types of cancer, especially those sensitive to hormones like breast or uterine cancer, due to concerns over how hormones could affect cancer cells.
Blood Clotting Issues:
If you have a history of blood clotting disorders or are at high risk for clots, you might not be a suitable candidate for HRT.
Uncontrolled High Blood Pressure:
People with uncontrolled hypertension should avoid HRT, as it could potentially worsen their condition.
Liver Disorders:
If you have severe liver problems, you might not be a good fit for HRT since it can affect liver function.
Heart Disease or Stroke History:
HRT could be risky for people who have had heart disease or a stroke, depending on the specific circumstances.
Risk Tolerance:
Some individuals are not willing to take on the potential risks of HRT, including possible side effects or long-term health issues.
Alternative Options:
Some people may prefer other methods, such as lifestyle changes or alternative therapies, to manage their symptoms without HRT.

Exploring HRT Costs in Depth
HRT Doctors Group and HRT Wellness offers a flat-fee pricing model to provide patients with a clear idea of what HRT treatment will cost. Regardless of the considerations and components below, our pricing model is always the same.
Types of Treatment:
Your choice of treatment type will not affect our flat-fee pricing or cost. Options like standard medication, bioidentical hormone replacement therapy (BHRT), or specialized programs are all priced the same.
Cost of Medication:
The expense of the actual medication will not impact our pricing. You’ll always know clearly what the HRT treatment will cost. Different types of medication, how they’re delivered (pills, patches, creams, injections), and the dosages will not impact our flat-fee pricing.
Treatment Duration:
At HRT Doctors Group/HRT Wellness, we have no contracts so you can start or stop whenever you’d like.
Expert Consultation:
Getting advice from qualified healthcare providers is essential. Our Doctors guidance will help tailor the treatment to your specific needs, and keep in mind that once you are a patient, consultations are included in the monthly fee. You do not pay any co-pays every time you need to meet with one of our Doctors, nurses, or medical staff.
Monitoring:
Regular check-ups and follow-up appointments are important for effective treatment. These appointments may include blood tests and evaluations, which are also included in the monthly flat-fee cost.
Meet Our Physicians
Our HRT Doctors are more than just medical experts; they are your allies in achieving optimal vitality and well-being. Let’s explore what sets them apart:
- Specialized Knowledge: each of our clinicians possesses specialized training in endocrine factors substituting therapy, comprehending the intricate aspects of endogenous balance.
- Empathy and Understanding: beyond their medical proficiency, our doctors approach their work with empathy and a profound understanding of the challenges you may face.
- Customized Care: one size doesn’t fit all in this. Our healthcare providers acknowledge that each individual is unique, and so are their endocrine needs.
- Cutting-Edge Expertise: the field of it is constantly evolving. Our doctors for hormone therapy stay at the forefront of medical advancements, ensuring you receive the latest, evidence-based management for the best possible outcomes.
Unlock Your Path to Wellness: Why Choose Our Online Clinic?
- Ease and Convenience:
Our online hormone replacement therapy (HRT) clinic makes expert healthcare easily accessible, right from the comfort of your home. There’s no need to travel long distances or rearrange your schedule. Our telemedicine approach ensures that quality healthcare is both convenient and easy to access.
- Personalized Care:
Your health journey is unique, and we get that. Especially when it comes to hormone therapy, a one-size-fits-all approach just won’t work. Our experienced healthcare providers will create a personalized treatment plan that’s tailored just for you.
- Reliable Expertise:
Your health deserves top-notch care, and our online clinic is staffed with highly qualified and experienced specialists. You can trust that you’re in good hands.
- Clear Communication and Education:
We believe in keeping you informed. Our clinic prioritizes transparent communication and patient education. Our doctors take the time to explain your treatment options, potential risks, and expected results in a way that’s easy to understand.
Ready to take the first step toward better health and happiness? Choose our online hormone therapy clinic to explore the benefits of hormone replacement therapy. We’re here to support you every step of the way on your journey to better health and well-being. Your wellness journey starts here.
Our board-certified HRT and TRT doctors use telemedicine to give convenient and more affordable access to Quality Care. Our practice addresses male patients. Our clinical practice can provide guidance to new patients seeking hormone therapy options or existing patients that are simply looking to switch to a more convenient telemedicine-based practice.
 Dr. Jay Flottman
Dr. Jay Flottman
 Dr. Melissa VanSickle
Dr. Melissa VanSickle
 Dr. Kevin Kargman
Dr. Kevin Kargman
 Dr. Peter Nwoke
Dr. Peter Nwoke
 Carleigh Ferrier PA-C
Carleigh Ferrier PA-C

The numerous health problems that men face as they age are treated in our medical programme. Our board-certified medical Doctors provide lab work, consultations, and evidence-based treatment at a fixed and affordable price.

We provide our patients a fixed price to accommodate their unique requirements. Our practice provides convenient care so that patients don’t have to sit in a waiting room. Patients in rural or urban areas across the US have access to specialised care via our telemedicine platform.
Our healthcare professional will collaborate with you to identify solutions for your health objectives, with a focus on your overall health and well-being. Our speciality is our commitment to you.

TRT & HRT
Are you ready to change your life by regaining your health? There is never a better moment to start managing your health than right NOW.
We have partnered with the nationwide laboratory, Quest Diagnostics, to provide accurate lab blood work testing and results.
Hypothyroidism, commonly referred to as an underactive thyroid, is a condition where the thyroid gland fails to produce sufficient amounts of thyroid hormones.
The Ultimate Guide to Bioidentical Hormones in Hormone Replacement Therapy
Testosterone, often hailed as the quintessential male hormone, plays a pivotal role in shaping male health and well-being.
Why Telemedicine Could Be a Valuable Option for Hormone Therapy
This article aims to provide a comprehensive understanding of why telemedicine could be an invaluable option for those seeking hormone therapy, addressing common queries and concerns while highlighting the potential for future advancements in this field.
Managing acne during testosterone replacement therapy
Introduction Acne, a common skin condition, knows no boundaries when it comes to age or gender. Traditionally associated with the turbulent years of adolescence, it can persist or even emerge for the first time in adulthood.
This clinical services set-up fee covers your initial electronic medical record review, Quest Diagnostics laboratory services to determine your current hormone levels and other key wellness attributes, and your first virtual doctor’s visit.
Provide our Board-Certified HRT Doctor’s with your medical history via our HIPAA-compliant platform.
We have partnered with the nationwide laboratory, Quest Diagnostics, to provide accurate lab testing and results. You can complete your blood test at any Quest Diagnostics nearby.
Our Board Certified HRT Doctors use telemedicine to give convenient and more affordable access to quality care. Our HRT physicians will consult with you to review your lab results, and discuss any current complaints, conditions, and symptoms . Based on the results of your consultation, the HRT Wellness physician will recommend the best treatment options.
Your treatment prescriptions will be shipped directly to you. Our Patient Care Team will provide in-depth assistance as you begin and progress through your treatment plan.