Balancing Act: Can Testosterone Therapy Fuel Uterine Cancer or Fight It?
Introduction: Understanding the Testosterone-Uterine Cancer Link
Testosterone therapy (TT) is a treatment that involves adding testosterone to the body to correct hormonal imbalances. It is often used in men with low testosterone, but some women also receive testosterone therapy for specific health conditions. In recent years, there has been growing interest in how testosterone therapy affects women, particularly in relation to hormone-sensitive conditions like uterine cancer. Some people worry that testosterone might increase the risk of uterine cancer, while others believe it may help prevent it. This article will explore the connection between testosterone therapy and uterine cancer, answering common questions based on scientific research.
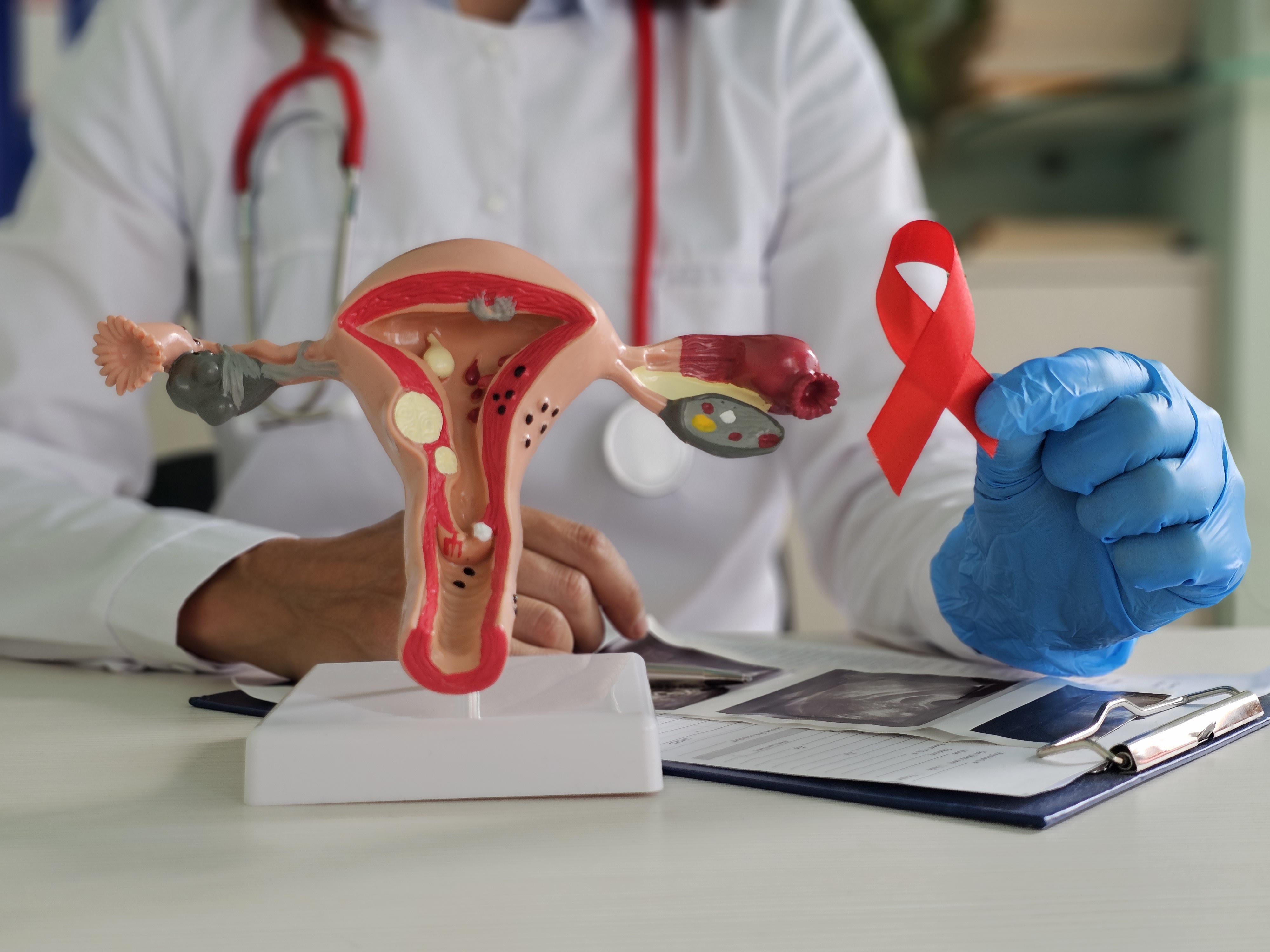
Uterine cancer is one of the most common cancers affecting women, particularly after menopause. It occurs when abnormal cells grow in the uterus, often starting in the endometrium, the inner lining of the uterus. There are two main types of uterine cancer: endometrial cancer, which is more common, and uterine sarcoma, which is rarer but more aggressive. Many factors influence the risk of uterine cancer, including age, obesity, genetics, and hormone levels. Estrogen, a key female hormone, is known to play a major role in the development of uterine cancer. Because testosterone can affect hormone levels in the body, some researchers are examining whether it has an impact on uterine cancer risk.
The relationship between testosterone therapy and uterine cancer is complex. Some studies suggest that testosterone may help balance estrogen levels and reduce the growth of the uterine lining, possibly lowering the risk of cancer. Other studies indicate that when testosterone converts to estrogen in the body, it may increase cancer risk. This debate makes it important for women, doctors, and researchers to understand the latest scientific evidence.
Testosterone therapy is prescribed to women for various reasons. Some women experience low testosterone due to menopause, removal of the ovaries, or medical conditions that affect hormone production. Symptoms of low testosterone in women can include fatigue, depression, low sex drive, and difficulty building muscle. In some cases, doctors prescribe testosterone therapy to help manage these symptoms. Additionally, transgender men may receive testosterone therapy as part of gender-affirming care. While testosterone can provide benefits, it is important to consider its effects on the body, including any potential risks related to the uterus.
The question of whether testosterone therapy increases or decreases the risk of uterine cancer is not easy to answer. Hormones work together in complex ways, and changing one hormone level can have effects on others. For example, in women, some testosterone naturally converts into estrogen through a process called aromatization. Since high estrogen levels are linked to a greater risk of endometrial cancer, this process could be a concern. However, some research suggests that testosterone might have protective effects by thinning the uterine lining, making it less likely for abnormal cells to grow.
This article aims to provide a clear and balanced review of the science behind testosterone therapy and uterine cancer. It will answer the most common questions people have about this topic, including whether testosterone therapy increases or decreases cancer risk, how it affects the uterine lining, and whether women on testosterone therapy need special cancer screenings. The goal is to provide accurate, research-based information so that women and healthcare providers can make informed decisions about testosterone therapy.
Because hormone therapy is a complex medical treatment, it is important to rely on scientific evidence rather than assumptions. Some people may believe that testosterone therapy is completely safe or completely dangerous, but the truth is likely somewhere in between. Research is still ongoing, and new findings continue to shape our understanding of how testosterone affects the uterus.
In the following sections, we will explore what causes uterine cancer, how testosterone interacts with female hormones, and what studies say about its impact on uterine health. We will also look at whether women on testosterone therapy should take extra precautions, such as regular screenings for uterine cancer. By the end of this article, readers will have a clearer understanding of the potential risks and benefits of testosterone therapy in relation to uterine cancer.
This is a subject that requires careful consideration, especially for women who are thinking about starting testosterone therapy. Any woman considering TT should have open discussions with her doctor about her personal risk factors, medical history, and overall health. As research continues, it is crucial to stay informed and make decisions based on the best available evidence.
What Is Testosterone Therapy and Why Is It Used?
Testosterone therapy (TT) is a medical treatment that supplements or replaces testosterone in people who have low levels of the hormone. Although testosterone is often thought of as a male hormone, it is also an important hormone in women. This section will explain what testosterone therapy is, how it works, and why it is prescribed for women.
What Is Testosterone?
Testosterone is a hormone that plays a key role in many body functions. It is part of a group of hormones called androgens. While men have higher levels of testosterone, women also produce it in smaller amounts. In women, testosterone is made in the ovaries, adrenal glands, and fat cells.
Testosterone helps regulate:
- Muscle strength and bone density – It helps maintain strong bones and muscle mass.
- Sex drive (libido) – It plays a role in sexual desire and arousal.
- Mood and energy levels – It can impact emotions, motivation, and fatigue.
- Cognitive function – Some studies suggest it affects memory and thinking.
- Metabolism and body fat – It may help with fat distribution and weight management.
When testosterone levels drop too low, it can lead to symptoms like fatigue, low libido, mood changes, muscle weakness, and weight gain.
Why Is Testosterone Therapy Used in Women?
Doctors may prescribe testosterone therapy for women who have low testosterone levels. While it is not as commonly used in women as in men, there are several conditions where TT may be beneficial.
- Menopause and Hormone Imbalance
As women age, their hormone levels change. Estrogen and progesterone levels decline during menopause, and testosterone levels can also drop. Some women experience symptoms such as low sex drive, fatigue, and mood swings. Testosterone therapy is sometimes used alongside estrogen therapy to help with these symptoms.
- Hypoactive Sexual Desire Disorder (HSDD)
HSDD is a condition where women experience a low sex drive that causes distress. It is not just a temporary loss of interest but an ongoing issue that affects daily life. Studies suggest that testosterone therapy can help improve sexual desire and satisfaction in women with HSDD.
- Surgical Menopause (Oophorectomy)
Women who have their ovaries removed (oophorectomy) experience a sudden drop in estrogen and testosterone levels. This can lead to symptoms like low energy, weight gain, and reduced sexual desire. Testosterone therapy may help restore hormonal balance.
- Adrenal Insufficiency
The adrenal glands produce small amounts of testosterone. In some conditions, such as Addison’s disease or adrenal fatigue, these glands do not produce enough hormones. This can lead to low testosterone symptoms. Testosterone therapy may be used to help manage these effects.
- Gender-Affirming Therapy
Transgender men (female-to-male individuals) often take testosterone as part of their gender transition. This helps promote physical changes like increased muscle mass, deepening of the voice, and body hair growth. In these cases, testosterone therapy is used at higher doses than in other conditions.
Forms of Testosterone Therapy
Testosterone therapy comes in different forms. The type of therapy used depends on a person’s medical history, lifestyle, and doctor’s recommendation.
- Gels and Creams
- Applied to the skin and absorbed into the bloodstream.
- Must be used daily.
- Can transfer to others through skin contact if not careful.
- Patches
- Worn on the skin and release testosterone slowly.
- Changed every day or every few days.
- Can cause skin irritation.
- Injections
- Given every few weeks or months.
- Can lead to hormone level fluctuations.
- Requires a healthcare provider or self-injection training.
- Pellets
- Small implants placed under the skin that release testosterone over months.
- Provides a steady hormone level.
- Requires a minor procedure to insert and remove.
Each method has its advantages and disadvantages, and not every method is suitable for every person.
How Is Testosterone Therapy Monitored?
Because testosterone therapy affects hormone balance, doctors monitor patients closely. Blood tests check testosterone levels, estrogen levels, and other factors like cholesterol and liver function. Side effects such as acne, hair growth, deepening voice, and mood changes are also monitored.
Doctors usually prescribe the lowest effective dose to reduce risks. Regular follow-ups help ensure that the therapy is working safely.
Testosterone therapy is used to treat low testosterone levels in women due to menopause, HSDD, adrenal conditions, and other medical issues. It comes in different forms, including gels, patches, injections, and pellets. While it can provide benefits such as improved energy, sex drive, and mood, it requires careful monitoring to avoid side effects.
Understanding why testosterone therapy is used and how it works is important for making informed healthcare decisions. The next section will discuss how testosterone therapy relates to uterine cancer, exploring whether it increases or decreases the risk.
What Causes Uterine Cancer?
Uterine cancer is one of the most common cancers in people with a uterus. It mainly affects people after menopause but can happen at any age. Understanding what causes uterine cancer is important for preventing and managing the disease. This section explains the two main types of uterine cancer, the role of hormones, and other risk factors that can contribute to its development.
Types of Uterine Cancer
There are two main types of uterine cancer:
- Endometrial Cancer
Endometrial cancer starts in the lining of the uterus, called the endometrium. It is the most common type of uterine cancer, making up about 90% of cases. This cancer often grows slowly and is usually found early because it causes abnormal bleeding. There are two main subtypes:
- Type 1 Endometrial Cancer (Estrogen-Dependent) – This is the most common type and grows when exposed to too much estrogen. It usually develops in people with obesity, hormone imbalances, or high estrogen levels.
- Type 2 Endometrial Cancer (Non-Estrogen Dependent) – This is less common but more aggressive. It does not depend on estrogen to grow and is harder to treat.
- Uterine Sarcoma
Uterine sarcoma is a rare but more aggressive cancer that starts in the muscle or connective tissue of the uterus. It does not always cause early symptoms, which makes it harder to detect.
How Hormones Play a Role in Uterine Cancer
Hormones are natural chemicals that help control different functions in the body. The two most important hormones for the uterus are estrogen and progesterone. These hormones work together to regulate the menstrual cycle, help with pregnancy, and keep the uterus healthy. However, when there is an imbalance—especially too much estrogen without enough progesterone—it can lead to cancer.
Estrogen and Uterine Cancer
Estrogen is a hormone that helps the uterus grow and shed its lining during each menstrual cycle. However, too much estrogen over a long period can make the endometrial lining grow too much, increasing the risk of cancer. Some causes of high estrogen levels include:
- Obesity – Fat cells produce estrogen. The more fat a person has, the more estrogen their body makes. This extra estrogen can cause the uterine lining to thicken, leading to cancer over time.
- Polycystic Ovary Syndrome (PCOS) – PCOS causes hormone imbalances, leading to higher estrogen levels and a greater risk of endometrial cancer.
- Hormone Replacement Therapy (HRT) – Taking estrogen alone (without progesterone) after menopause can increase the risk of uterine cancer. This is why doctors often recommend using progesterone along with estrogen.
- Early Menstruation and Late Menopause – If a person starts their period before age 12 or goes through menopause after age 55, they are exposed to estrogen for a longer time, increasing their risk.
Progesterone’s Protective Role
Progesterone is another important hormone that balances the effects of estrogen. It helps thin the uterine lining and prevents it from growing too much. If a person has low progesterone levels, they may develop a condition called endometrial hyperplasia, which can turn into cancer. People with PCOS, obesity, or irregular periods often have lower progesterone levels.
Other Risk Factors for Uterine Cancer
Besides hormones, other factors can contribute to the development of uterine cancer.
Genetics and Family History
Some people inherit gene mutations that increase their risk of uterine cancer. A condition called Lynch syndrome raises the risk of several cancers, including uterine cancer. If a close family member has had uterine, colon, or ovarian cancer, the risk may be higher.
Obesity and Metabolic Syndrome
Obesity is one of the biggest risk factors for uterine cancer. Fat cells produce extra estrogen, which can make the endometrial lining grow too much. Metabolic syndrome, a group of conditions including high blood sugar, high blood pressure, and excess body fat, also increases the risk of uterine cancer.
Diabetes and Insulin Resistance
People with type 2 diabetes or insulin resistance have a higher risk of uterine cancer. High insulin levels can lead to more estrogen production and increase cancer risk.
Tamoxifen Use
Tamoxifen is a drug used to treat breast cancer, but it can also act like estrogen in the uterus. Long-term use of tamoxifen may increase the risk of uterine cancer. If a person needs tamoxifen, their doctor will monitor them for any signs of uterine cancer.
Radiation Therapy to the Pelvis
People who have had radiation therapy to treat other cancers in the pelvic area may have a higher risk of developing uterine sarcoma later in life.
How to Reduce the Risk of Uterine Cancer
Although some risk factors cannot be changed (like genetics), there are ways to lower the risk of uterine cancer:
- Maintain a Healthy Weight – Losing weight can lower estrogen levels and reduce cancer risk.
- Manage Hormones Carefully – If taking hormone replacement therapy, use progesterone along with estrogen to protect the uterus.
- Monitor Blood Sugar and Insulin Levels – Keeping blood sugar levels stable can lower the risk of metabolic syndrome and diabetes, which are linked to uterine cancer.
- Use Birth Control Pills – Some studies show that using birth control pills with estrogen and progesterone can lower the risk of endometrial cancer.
- Regular Checkups and Screening – Seeing a doctor for regular exams can help catch any early signs of uterine cancer.
Uterine cancer is caused by a combination of hormonal imbalances, genetic factors, obesity, and other health conditions. Too much estrogen without enough progesterone is one of the biggest risk factors, as it can make the uterine lining grow too much. Other factors like obesity, diabetes, and tamoxifen use can also increase the risk.
Understanding these causes can help people take steps to reduce their risk, such as maintaining a healthy weight, balancing hormone levels, and going for regular medical checkups. By being aware of the factors that contribute to uterine cancer, individuals can work with their doctors to make informed health decisions.
Does Testosterone Therapy Increase the Risk of Uterine Cancer?
Testosterone therapy (TT) is used by some women to treat hormone imbalances, menopause symptoms, or conditions like hypoactive sexual desire disorder. It is also used by transgender men as part of gender-affirming hormone therapy. However, many people wonder if taking testosterone can increase the risk of uterine cancer. The answer is complex because testosterone interacts with other hormones in the body, especially estrogen and progesterone, which play a key role in uterine health.
What Does Research Say About Testosterone and Uterine Cancer?
So far, there is no strong scientific evidence proving that testosterone therapy directly increases the risk of uterine cancer. Most studies on hormone-related cancers focus on estrogen and progesterone because they are the primary hormones that influence the uterine lining. However, some researchers have tried to understand how testosterone affects the uterus.
- Limited Studies on Women: Research on testosterone therapy and uterine cancer in women is limited. Most studies have been done on animals or in lab settings. There are few long-term studies on how TT affects the uterus in humans.
- Mixed Results in Existing Research: Some studies suggest that testosterone might help prevent uterine cancer by stopping the growth of the uterine lining, while others suggest that it could increase cancer risk if the body converts too much testosterone into estrogen.
Since the research is still developing, doctors do not have a definite answer. However, they do know that hormone balance is important when it comes to cancer risk.
How Does Testosterone Interact With Estrogen and Progesterone?
The uterus is very sensitive to hormone changes. Estrogen and progesterone help regulate the growth and shedding of the uterine lining during the menstrual cycle. An imbalance in these hormones can lead to problems such as excessive growth of the lining (endometrial hyperplasia), which can increase the risk of uterine cancer.
Testosterone does not directly cause uterine cancer, but it interacts with estrogen and progesterone in different ways:
- Testosterone Can Convert to Estrogen: The body naturally converts some testosterone into estrogen through a process called aromatization. This means that taking testosterone could lead to an increase in estrogen levels, which might promote the growth of the uterine lining and increase cancer risk.
- Testosterone Can Counteract Estrogen’s Effects: At the same time, testosterone can also have an anti-estrogenic effect. It can block some of the effects of estrogen on the uterus, preventing excessive growth of the uterine lining. Some researchers believe this might actually reduce the risk of uterine cancer.
- The Role of Progesterone: Progesterone balances the effects of estrogen by thinning the uterine lining. If a woman is taking testosterone without progesterone, and the body is converting some testosterone into estrogen, the risk of endometrial hyperplasia might increase.
Because of these complex interactions, the impact of testosterone therapy on the uterus depends on a person’s hormone levels, genetics, and medical history.
Does the Dose and Duration of Testosterone Therapy Matter?
The risk of uterine cancer may depend on how much testosterone a person takes and for how long.
- Higher Doses Might Increase Aromatization: If a person takes very high doses of testosterone, more of it may convert into estrogen. This could cause the uterine lining to grow abnormally, increasing the risk of endometrial hyperplasia or, in rare cases, cancer.
- Long-Term Use Without Monitoring: If someone is on testosterone therapy for many years without regular monitoring, they may not notice changes in the uterine lining until symptoms appear. Early detection is key to preventing complications.
Doctors often recommend regular check-ups, including ultrasounds and hormone level testing, for people taking testosterone therapy. This helps ensure that the uterine lining stays healthy.
Are Certain Groups at Higher Risk?
Some people may have a higher risk of uterine cancer if they use testosterone therapy, including:
- Women with a History of Endometrial Hyperplasia: If someone already has a condition where the uterine lining grows too thick, extra hormones could make the problem worse.
- People Who Are Overweight or Obese: Fat tissue can convert testosterone into estrogen, increasing overall estrogen levels in the body. This may raise the risk of uterine cancer.
- People with Polycystic Ovary Syndrome (PCOS): Many people with PCOS already have high levels of testosterone and irregular hormone patterns. Adding extra testosterone might further disrupt the balance and affect the uterine lining.
If a person falls into one of these categories, they should have careful medical supervision while on testosterone therapy.
There is no clear evidence that testosterone therapy directly causes uterine cancer. However, because testosterone can be converted into estrogen, it may still affect the uterine lining, especially in certain individuals. The impact of testosterone therapy on the uterus depends on many factors, including hormone levels, dose, and medical history.
Doctors recommend regular monitoring, including hormone testing and ultrasounds, for people using testosterone therapy. This helps detect any changes in the uterine lining early and lowers the risk of complications.
For those considering TT, discussing risks and benefits with a healthcare provider is essential. Each person’s body reacts differently to hormone therapy, so a personalized approach is the safest way to balance the benefits of testosterone while protecting uterine health.
Can Testosterone Therapy Help Prevent Uterine Cancer?
Testosterone therapy (TT) is commonly used to treat symptoms of low testosterone in women, such as fatigue, low libido, and muscle loss. Some researchers have suggested that TT might have a protective effect against uterine cancer, but this idea is still being studied. This section explores whether testosterone can help prevent uterine cancer by looking at its effects on the endometrium (the lining of the uterus), its role in balancing estrogen, and research findings on this topic.
Testosterone’s Potential Protective Effects on the Endometrium
The endometrium is the inner lining of the uterus. It goes through changes during a woman's menstrual cycle, thickening in response to estrogen and shedding during menstruation. When a woman goes through menopause, estrogen levels decrease, which can cause the endometrium to thin. However, if estrogen levels remain high without enough progesterone to balance them, the endometrial lining can grow too thick. This condition, called endometrial hyperplasia, increases the risk of uterine cancer.
Some studies suggest that testosterone may help prevent excessive growth of the endometrium. Researchers believe that testosterone has anti-proliferative effects, meaning it may help slow down or stop abnormal cell growth in the uterine lining. This could potentially lower the risk of developing uterine cancer, particularly in women who have high estrogen levels or are on estrogen therapy without progesterone.
How Testosterone Helps Balance Estrogen
Estrogen is a key hormone in the female body, but too much of it over time can increase the risk of uterine cancer. Many cases of uterine cancer, particularly endometrial cancer, are linked to unopposed estrogen exposure. This means there is an excess of estrogen without enough progesterone to counteract its effects.
Testosterone plays an indirect role in controlling estrogen’s impact on the uterus in two ways:
- Reducing Estrogen-Driven Growth: Some research suggests that testosterone can reduce the effects of estrogen on the endometrial lining by blocking estrogen receptors. When estrogen receptors are blocked, estrogen cannot stimulate as much endometrial growth, which may help lower the risk of abnormal cell changes.
- Competing with Estrogen at the Cellular Level: Testosterone may also compete with estrogen in certain tissues, including the uterus. This means that when testosterone levels are higher, estrogen may have less influence on the growth of the endometrial lining.
For these reasons, some scientists believe that testosterone could act as a natural counterbalance to estrogen, helping to reduce the risk of endometrial hyperplasia and potentially lowering the chances of developing uterine cancer.
Does Testosterone Help Reduce Endometrial Hyperplasia?
Endometrial hyperplasia is a condition where the endometrium becomes too thick, which can lead to uterine cancer if left untreated. Women who have high estrogen levels, are overweight, or take estrogen therapy without progesterone are at greater risk.
Some research suggests that testosterone may help thin the endometrial lining, reducing the likelihood of hyperplasia. A few small studies have found that women who take testosterone therapy along with estrogen therapy may have a lower risk of endometrial thickening compared to those who take estrogen alone. However, the evidence is still limited, and more research is needed to confirm these findings.
Doctors may monitor endometrial thickness in women taking TT, especially those who are postmenopausal. A transvaginal ultrasound can help measure the endometrium’s thickness to determine if there are any unusual changes. If the endometrial lining remains thin while on TT, it may suggest that testosterone is not contributing to endometrial hyperplasia.
What Does Research Say About Testosterone and Uterine Cancer Risk?
Research on testosterone therapy and uterine cancer is still evolving, and there is no clear answer yet. However, some early findings suggest that TT does not appear to increase the risk of uterine cancer and may even help lower the risk.
- A few small studies have found that women using testosterone therapy did not have higher rates of endometrial cancer compared to those who did not use testosterone.
- Some studies suggest that testosterone might have a protective effect by reducing estrogen-driven endometrial growth.
- However, other researchers caution that testosterone can convert to estrogen in the body through a process called aromatization. This means that in some women, high doses of testosterone could still lead to increased estrogen levels, potentially raising the risk of endometrial hyperplasia.
Since the research is still inconclusive, doctors typically take a case-by-case approach when prescribing TT to women, especially those with risk factors for uterine cancer.
Who Might Benefit from Testosterone’s Protective Effects?
Women who might benefit from testosterone’s potential protective effects include:
- Women on Estrogen Therapy: Those using estrogen replacement therapy (ERT) without progesterone may be at higher risk of endometrial hyperplasia. Adding testosterone to their treatment may help balance estrogen’s effects.
- Women with Polycystic Ovary Syndrome (PCOS): PCOS is a condition linked to both high estrogen levels and an increased risk of endometrial hyperplasia. Some doctors believe that testosterone therapy could help regulate hormone levels in these women.
- Postmenopausal Women: After menopause, estrogen levels drop, but if a woman takes hormone replacement therapy (HRT), the risk of endometrial thickening may increase. Testosterone might help counteract this effect.
However, more studies are needed before doctors can confidently recommend TT as a preventive treatment for uterine cancer.
While there is some evidence suggesting that testosterone may help prevent uterine cancer by balancing estrogen and reducing endometrial growth, the research is not yet strong enough to make a clear recommendation. Some studies indicate that testosterone might lower the risk of endometrial hyperplasia, while others caution that it could be converted into estrogen and contribute to the problem.
For now, women considering TT should speak with their doctor about their personal health history and risk factors. More research is needed to fully understand whether testosterone therapy can be used as a protective treatment against uterine cancer. Until then, regular monitoring and individualized medical care remain the best approach.
How Does Testosterone Interact with Estrogen and Progesterone in the Uterus?
Hormones play a major role in how the uterus functions. The balance of estrogen, progesterone, and testosterone affects many aspects of female health, including the risk of uterine cancer. Testosterone therapy (TT) is sometimes used in women to help with hormone imbalances, but many people wonder how it interacts with estrogen and progesterone inside the body. Does it increase or decrease the risk of uterine problems? To understand this, we need to look at how these hormones work together.
The Role of Estrogen in the Uterus
Estrogen is one of the most important hormones for the uterus. It helps build up the uterine lining (endometrium) each month. This is important for pregnancy, but when estrogen levels are too high for a long time, it can cause problems. If the endometrium grows too much, a condition called endometrial hyperplasia can develop. This can sometimes lead to endometrial cancer, the most common type of uterine cancer.
When women go through menopause, their estrogen levels drop. This can cause symptoms like hot flashes, vaginal dryness, and bone loss. Some women take hormone replacement therapy (HRT) to replace estrogen and reduce these symptoms. However, taking estrogen alone can increase the risk of uterine cancer. That’s why doctors often prescribe progesterone along with estrogen to help protect the uterus.
The Role of Progesterone in the Uterus
Progesterone is another key hormone that affects the uterus. It balances the effects of estrogen by thinning the uterine lining and stopping it from growing too much. When estrogen and progesterone are balanced, the uterus stays healthy. But if progesterone is too low, estrogen can take over and cause excessive growth of the endometrium. This increases the risk of abnormal cells forming, which can lead to cancer.
How Does Testosterone Fit Into This?
Testosterone is often thought of as a male hormone, but women also produce it in small amounts. It plays a role in muscle strength, energy, mood, and sex drive. Some women use testosterone therapy (TT) if their levels are too low due to menopause, medical conditions, or hormone imbalances. But how does testosterone affect the uterus?
Testosterone interacts with both estrogen and progesterone in the body, and its effects can be complex. Here’s how:
- Testosterone Can Be Converted Into Estrogen
- The body naturally changes some testosterone into estradiol, a form of estrogen, through a process called aromatization.
- This means that taking extra testosterone can sometimes increase estrogen levels.
- Higher estrogen levels can lead to endometrial thickening and possibly increase the risk of uterine hyperplasia or cancer.
- Testosterone May Counteract Some Effects of Estrogen
- Some research suggests that testosterone might act against estrogen in certain ways.
- It may reduce the growth of the endometrial lining, which could help lower the risk of uterine cancer.
- This effect is not fully understood and depends on the dosage and form of testosterone therapy.
- Testosterone May Act Like Progesterone in Some Cases
- Some studies suggest that testosterone might work similarly to progesterone by keeping the endometrial lining thin.
- This could be helpful for women at risk of estrogen dominance (when estrogen levels are too high compared to progesterone).
- However, this effect is not strong enough to replace progesterone completely.
Does Testosterone Affect Premenopausal and Postmenopausal Women Differently?
Yes, testosterone’s effects can vary depending on age and hormonal status.
- Premenopausal Women:
- These women still have natural estrogen and progesterone cycles.
- Adding testosterone may slightly increase estrogen levels due to aromatization.
- If estrogen levels rise too much, the endometrial lining could thicken, leading to a higher risk of irregular bleeding or hyperplasia.
- Postmenopausal Women:
- They have lower natural estrogen and progesterone levels.
- Testosterone therapy might help prevent bone loss, low libido, and muscle weakness.
- If not monitored properly, testosterone could be converted into estrogen and cause unwanted endometrial growth.
What Happens When Estrogen, Progesterone, and Testosterone Are Out of Balance?
If any of these three hormones are too high or too low, problems can occur:
- Too much estrogen (without progesterone or testosterone balance)
- Can lead to excess endometrial growth and increase the risk of cancer.
- Too little estrogen (with too much testosterone)
- Can cause vaginal dryness, mood swings, and bone loss.
- Too much testosterone (especially if converted into estrogen)
- Might cause weight gain, hair loss, or irregular bleeding.
- Balanced estrogen, progesterone, and testosterone
- Helps keep the uterus healthy and stable.
What Should Women on Testosterone Therapy Be Aware Of?
Women who take testosterone therapy should be closely monitored by their doctors. Important steps include:
- Regular hormone level checks to ensure estrogen, progesterone, and testosterone are balanced.
- Ultrasound exams to check endometrial thickness, especially in postmenopausal women.
- Discussing symptoms with a doctor, such as irregular bleeding or pelvic pain, which might signal hormonal imbalances.
Testosterone does not act alone in the body—it interacts with estrogen and progesterone in complex ways. While some studies suggest it might help thin the uterine lining, others show it can increase estrogen levels through aromatization, possibly raising the risk of endometrial hyperplasia. The effects depend on individual hormone levels, dosage, and duration of use. Women considering testosterone therapy should work closely with their healthcare providers to ensure hormone balance and uterine health are maintained.
Is Testosterone Therapy Safe for Women with a History of Uterine Cancer?
Women who have had uterine cancer often have concerns about whether taking testosterone therapy (TT) is safe. Testosterone therapy is sometimes used to help women manage symptoms like low energy, reduced muscle mass, or low sex drive, especially after menopause or certain medical treatments. However, since uterine cancer is often linked to hormones, there is a valid concern about whether testosterone could increase the risk of cancer coming back.
Understanding Uterine Cancer and Hormones
Uterine cancer is mainly of two types:
- Endometrial Cancer: This type starts in the lining of the uterus (endometrium). It is the most common type and is often linked to hormone imbalances, especially too much estrogen without enough progesterone to balance it.
- Uterine Sarcoma: A rare and more aggressive type that starts in the muscle or tissue of the uterus. This type is less connected to hormones.
Because many cases of endometrial cancer are caused by excess estrogen, doctors often focus on hormone balance when considering treatment options for survivors.
How Testosterone Therapy Works
Testosterone is a hormone that plays a role in muscle strength, bone health, mood, and sexual function. Even though it is often called a "male hormone," women also produce small amounts of testosterone naturally in their ovaries and adrenal glands.
Testosterone therapy is sometimes used in women who have:
- Low testosterone levels due to menopause or medical conditions.
- Undergone surgery to remove their ovaries (which produce both estrogen and testosterone).
- Symptoms like fatigue, low libido, or muscle weakness.
Testosterone can be given as creams, gels, injections, or pellets implanted under the skin.
Could Testosterone Therapy Lead to Uterine Cancer Recurrence?
The big question for women who have had uterine cancer is whether testosterone therapy could make the cancer come back. The answer is not simple because research on this topic is still limited. However, there are some key points to consider:
- Testosterone Can Convert into Estrogen
One of the biggest concerns with testosterone therapy is that some of it can turn into estrogen in the body. This process is called aromatization and happens more in fat tissue. Since estrogen is known to fuel the growth of some uterine cancers, this could be a risk factor for recurrence in women who have had hormone-sensitive cancers.
- Testosterone May Have Protective Effects
On the other hand, some studies suggest that testosterone itself may help counteract the effects of estrogen by preventing the overgrowth of the uterine lining (endometrial hyperplasia). Some research even suggests that testosterone might have anti-cancer properties, though this is not yet proven in large studies.
- The Role of Progesterone in Balancing Hormones
For women who still have a uterus and are taking any form of hormone therapy, doctors often recommend adding progesterone to help protect the uterine lining. Progesterone helps keep the endometrial cells from growing too much, which reduces the risk of cancer returning. However, whether testosterone alone has a similar protective effect is still unclear.
Medical Guidelines and Expert Recommendations
Because the research on testosterone therapy and uterine cancer recurrence is still evolving, most doctors follow a cautious approach when considering TT for cancer survivors. Here are some general recommendations:
- Consult with a Specialist
Women with a history of uterine cancer should always discuss testosterone therapy with an oncologist (cancer doctor) and an endocrinologist (hormone specialist) before starting treatment. A personalized approach is important because each case is different. - Regular Cancer Monitoring
If a woman with a history of uterine cancer decides to use TT, regular monitoring is essential. This may include:- Pelvic ultrasounds to check for changes in the endometrial lining.
- Blood tests to monitor hormone levels and ensure testosterone is not turning into too much estrogen.
- Biopsies if there are any unusual symptoms, like abnormal bleeding.
- Choosing the Right Type and Dose of Testosterone
- Lower doses of testosterone may be safer than higher doses.
- Non-aromatizing forms of testosterone (which do not convert easily to estrogen) may be preferable.
- Some doctors recommend combined therapy with progesterone to help balance hormones.
- Lifestyle Factors to Reduce Cancer Risk
Women who take testosterone therapy should also focus on lifestyle choices that help reduce cancer risk, such as:- Maintaining a healthy weight to prevent excess fat tissue from converting testosterone into estrogen.
- Eating a balanced diet rich in vegetables, lean proteins, and whole grains to support hormone balance.
- Engaging in regular exercise to improve metabolism and overall health.
Should Women with a History of Uterine Cancer Take Testosterone Therapy?
At this time, there is no clear answer because more research is needed. Some doctors believe that low-dose testosterone therapy may be safe for certain women, especially those who are closely monitored. Others recommend avoiding it altogether in women with a history of hormone-sensitive uterine cancer, just to be on the safe side.
Women considering TT should carefully weigh the potential benefits (such as improved energy, mood, and libido) against the possible risks (such as increased estrogen levels and cancer recurrence).
For women with a history of uterine cancer, the decision to use testosterone therapy should be made with careful medical guidance. Because there is still uncertainty about whether TT increases the risk of cancer recurrence, women should work closely with their doctors to create a plan that balances hormone therapy with cancer safety.
Regular check-ups, close monitoring, and a healthy lifestyle can help reduce risks while still addressing symptoms that testosterone therapy might improve. The most important thing is to have an open conversation with a healthcare provider before starting or continuing testosterone therapy.
How Does Testosterone Therapy Affect Endometrial Thickness?
Testosterone therapy (TT) is often prescribed for women with low testosterone levels due to aging, menopause, or medical conditions. However, one major concern is whether TT affects the lining of the uterus, known as the endometrium. The endometrial thickness is important because an abnormally thick lining can increase the risk of endometrial hyperplasia and, in some cases, endometrial cancer. This section will explain how TT may influence the endometrium, how it compares to other hormone therapies, and what monitoring is needed.
What Is Endometrial Thickness and Why Does It Matter?
The endometrium is the inner lining of the uterus. Its thickness changes throughout a woman's menstrual cycle due to the effects of estrogen and progesterone.
- In premenopausal women, the endometrium thickens during the first half of the cycle due to rising estrogen levels. After ovulation, progesterone helps prepare the lining for pregnancy. If no pregnancy occurs, the lining sheds during menstruation.
- In postmenopausal women, the endometrium is usually thinner because of lower hormone levels. If it becomes abnormally thick, it could signal a problem, such as endometrial hyperplasia or cancer.
Doctors measure endometrial thickness using transvaginal ultrasound. In postmenopausal women, an endometrial thickness greater than 4 mm may require further evaluation to rule out cancer or other abnormalities.
Can Testosterone Therapy Thicken or Thin the Endometrium?
The effect of testosterone on the endometrium depends on several factors, including how much testosterone is used, how the body metabolizes it, and whether estrogen is also present.
- Testosterone’s Direct Effect on the Endometrium
Testosterone has androgenic properties, meaning it acts as a male hormone. Unlike estrogen, it does not directly stimulate endometrial growth. Some studies suggest that TT can actually cause endometrial thinning by counteracting estrogen’s effects.
- Endometrial atrophy (thinning): Some researchers believe that TT, especially at high doses, can lead to a thinner endometrium because it reduces estrogen’s ability to stimulate growth. This could lower the risk of endometrial hyperplasia or cancer.
- Endometrial hyperplasia (thickening): In some cases, testosterone can convert to estrogen in a process called aromatization. This is more likely in women who have higher body fat, as fat cells help convert testosterone into estrogen. Increased estrogen levels can thicken the endometrium, especially in women who are also taking estrogen therapy.
- Differences Between Testosterone Therapy and Estrogen Therapy
Estrogen therapy (ET) is often prescribed to postmenopausal women to relieve symptoms such as hot flashes and vaginal dryness. However, estrogen can cause the endometrial lining to thicken, increasing the risk of hyperplasia and cancer if not balanced with progesterone.
- Testosterone vs. Estrogen Alone: Unlike estrogen, testosterone does not directly stimulate endometrial growth, and some studies suggest it may even have a protective effect.
- Testosterone vs. Combined Estrogen-Progesterone Therapy: Many postmenopausal women take a combination of estrogen and progesterone to prevent endometrial thickening. When testosterone is added to this combination, its impact on the endometrium is less clear and may depend on individual factors.
Does the Type of Testosterone Therapy Matter?
Different forms of testosterone therapy may have different effects on the endometrium.
- Injectable Testosterone: This method delivers higher testosterone levels into the body, which may increase the chance of aromatization (conversion to estrogen), potentially affecting endometrial thickness.
- Testosterone Gels and Patches: These provide steady levels of testosterone and may have less impact on estrogen levels.
- Testosterone Pellets: These are inserted under the skin and release testosterone slowly over time. Some studies suggest they may reduce estrogen production and help keep the endometrium thin.
The effects of TT on the endometrium can vary from person to person. Factors such as body weight, metabolism, and whether a woman is also taking estrogen or progesterone can influence how TT affects the uterus.
How Should Women on Testosterone Therapy Monitor Endometrial Thickness?
Since TT can have different effects on the uterus, it is important for women to have regular monitoring.
- Transvaginal Ultrasound: This is the most common way to check endometrial thickness. It is especially recommended for women who experience abnormal bleeding while on TT.
- Endometrial Biopsy: If an ultrasound shows thickening or abnormalities, a biopsy may be needed to check for hyperplasia or cancer.
- Hormone Level Testing: Monitoring testosterone, estrogen, and progesterone levels can help determine if hormonal balance is being maintained.
Women who have a history of endometrial hyperplasia, polycystic ovary syndrome (PCOS), or obesity may require closer monitoring while on TT.
When Should a Woman on Testosterone Therapy Seek Medical Attention?
Any woman on TT should consult a doctor if she experiences:
- Unexplained vaginal bleeding: This could be a sign of endometrial changes and should be evaluated immediately.
- Pelvic pain or pressure: This could indicate uterine abnormalities.
- Unusual discharge or other symptoms: These may need further testing to rule out infections or other conditions.
If a woman has risk factors for uterine cancer, such as a family history, obesity, or diabetes, she should discuss the risks and benefits of TT with her doctor before starting therapy.
The relationship between testosterone therapy and endometrial thickness is complex. While testosterone may thin the endometrium in some cases, it can also lead to increased estrogen levels, which might cause thickening. The effects depend on the type of TT, the individual’s hormone metabolism, and whether other hormones like estrogen or progesterone are also present.
Regular monitoring with ultrasounds and hormone level testing can help detect any potential issues early. Women who experience abnormal bleeding or other concerning symptoms should seek medical evaluation. More research is needed to fully understand how TT impacts endometrial health, but for now, careful monitoring and individualized treatment remain the best approach.
What Are the Symptoms of Uterine Cancer, and Can Testosterone Therapy Mask or Mimic Them?
Uterine cancer, which mainly includes endometrial cancer and uterine sarcoma, can have symptoms that overlap with hormonal changes caused by testosterone therapy (TT). This overlap can make it challenging to recognize early warning signs of cancer in women who are taking testosterone. In this section, we will discuss the common symptoms of uterine cancer, how TT may affect these symptoms, and when to seek medical advice.
Common Symptoms of Uterine Cancer
Uterine cancer often develops in the lining of the uterus, called the endometrium. The most common warning signs include:
- Abnormal vaginal bleeding
- This is the most common symptom of uterine cancer.
- Bleeding may happen between periods, after menopause, or be heavier than normal.
- Any bleeding after menopause is considered abnormal and should be checked by a doctor.
- Pelvic pain or discomfort
- Some women with uterine cancer experience persistent pain, cramping, or pressure in the lower abdomen or pelvis.
- This pain is usually not linked to menstruation and may become worse over time.
- Unusual vaginal discharge
- Vaginal discharge may appear watery, pink, or dark brown.
- It may have a foul smell in some cases.
- Even if the discharge is not bloody, any sudden change should be evaluated.
- Pain during urination or bowel movements
- Uterine tumors may press on the bladder or intestines, leading to pain, frequent urination, constipation, or bloating.
- Unexplained weight loss or fatigue
- Losing weight without trying and feeling constantly tired can be signs of advanced cancer.
- A mass or swelling in the abdomen
- In rare cases, a growing tumor may cause visible swelling in the lower belly.
These symptoms can also be caused by non-cancerous conditions like fibroids, infections, or hormonal imbalances. However, any persistent or unusual symptoms should be discussed with a healthcare provider.
Can Testosterone Therapy Mimic Uterine Cancer Symptoms?
Testosterone therapy affects hormone levels in women, which can lead to changes in the reproductive system. Some of these changes overlap with uterine cancer symptoms, making it difficult to tell them apart.
- Irregular vaginal bleeding
- TT can cause irregular spotting or bleeding, especially during the first few months of treatment.
- This is because testosterone can be converted into estrogen in the body, which may stimulate the endometrial lining.
- Women on TT who experience persistent or heavy bleeding should see a doctor to rule out serious conditions.
- Pelvic discomfort
- Some women using testosterone report pelvic discomfort, bloating, or pressure.
- These symptoms may be due to hormonal changes rather than cancer.
- Changes in vaginal discharge
- TT may lead to vaginal dryness, irritation, or changes in discharge due to reduced estrogen levels.
- While this is different from cancer-related discharge, any unusual discharge with odor or blood should be checked.
- Urinary symptoms
- Testosterone can cause increased urination, mild discomfort, or urgency as hormone levels adjust.
- These symptoms may resemble bladder problems linked to uterine cancer.
- Weight changes and fatigue
- TT may increase muscle mass and reduce fat, but some women feel tired or experience changes in appetite.
- Unexplained weight loss should still be investigated, as it is a potential sign of cancer.
Because TT can cause symptoms similar to uterine cancer, it is important to track any changes and discuss them with a doctor.
When to Seek Medical Attention
It is crucial to know when symptoms require urgent medical evaluation. See a doctor if you experience:
- Any vaginal bleeding after menopause
- Heavy or prolonged bleeding between periods
- Persistent pelvic pain or pressure that does not go away
- Unusual vaginal discharge that lasts more than a few weeks
- Pain or discomfort during urination or bowel movements
- Unexplained weight loss, fatigue, or abdominal swelling
Even if TT is causing some of these symptoms, doctors can perform tests to rule out cancer and ensure that the symptoms are not caused by a serious underlying condition.
How Uterine Cancer is Diagnosed
If you have concerning symptoms, your doctor may recommend the following tests:
- Pelvic Exam – A doctor checks for lumps or abnormalities in the uterus and surrounding organs.
- Transvaginal Ultrasound (TVUS) – A painless imaging test that looks at the thickness of the endometrial lining.
- Endometrial Biopsy – A small sample of the uterine lining is taken and tested for cancer cells.
- Hysteroscopy – A small camera is inserted into the uterus to look for abnormal tissue.
- MRI or CT Scan – These imaging tests may be used to check for cancer spread in advanced cases.
Testosterone therapy can cause symptoms that overlap with uterine cancer warning signs, including irregular bleeding, pelvic discomfort, and changes in vaginal discharge. While these symptoms may be side effects of hormone therapy, they should never be ignored. If you are on TT and experience any persistent or unusual symptoms, seek medical advice as soon as possible. Regular monitoring and early detection are key to preventing serious health issues.
By staying informed and having open communication with your healthcare provider, you can safely manage your health while using testosterone therapy.
Should Women on Testosterone Therapy Undergo Special Cancer Screenings?
Testosterone therapy (TT) is commonly prescribed for women experiencing hormone imbalances, menopause symptoms, or gender-affirming care. However, given the role of hormones in many cancers, especially uterine cancer, a major concern is whether women on TT should have special cancer screenings. This section will explain the importance of screening, what tests may be needed, and how often they should be done.
Why Screening Is Important for Women on Testosterone Therapy
Cancer screening is a key part of preventive healthcare. The main goal of cancer screening is to find cancer early when it is easier to treat. Uterine cancer, also called endometrial cancer, often develops due to changes in hormone levels. Since testosterone can influence estrogen and progesterone levels in the body, it is important to monitor the uterus for any changes.
Women using TT may need special screening because:
- Hormone Changes Affect the Uterus – Testosterone therapy can change how the uterine lining (endometrium) grows. If the balance between testosterone, estrogen, and progesterone is not right, the endometrium may become too thick. A thickened endometrium can increase the risk of cancer.
- Testosterone Can Convert to Estrogen – In the body, testosterone can turn into estrogen through a process called aromatization. If too much estrogen is produced, it may increase the risk of endometrial hyperplasia (overgrowth of the uterine lining), which can sometimes lead to cancer.
- Symptoms Can Be Confusing – Women on TT might experience irregular bleeding, spotting, or other changes in menstrual cycles. These symptoms could be due to TT or could be warning signs of uterine cancer. Screening can help find the cause.
What Screening Tests Are Recommended?
Several medical tests can help check for signs of uterine cancer. The specific tests recommended depend on a woman’s medical history, symptoms, and risk factors.
- Pelvic Exam
- A doctor examines the uterus, ovaries, and surrounding areas to check for abnormalities.
- While a pelvic exam does not directly detect uterine cancer, it can help find unusual growths or pain that may require further testing.
- Transvaginal Ultrasound (TVUS)
- This test uses sound waves to create images of the uterus.
- Doctors use it to measure the thickness of the endometrium. A thicker lining may suggest an increased risk of cancer.
- It is a non-invasive test and is often used for women with unusual bleeding.
- Endometrial Biopsy
- A small sample of the uterine lining is collected and examined under a microscope.
- This is one of the best ways to detect early-stage uterine cancer.
- It is usually done if a woman has abnormal bleeding or if the ultrasound shows thickening of the endometrium.
- Hysteroscopy
- A thin, lighted tube is inserted into the uterus to allow doctors to see inside.
- It can help diagnose endometrial polyps, fibroids, or other changes that may be linked to cancer.
- If something unusual is found, a biopsy may also be performed at the same time.
How Often Should Women on Testosterone Therapy Be Screened?
The frequency of screenings depends on a woman’s individual health history, age, and symptoms. General guidelines include:
- Women With No Symptoms
- Routine pelvic exams should be done yearly.
- A transvaginal ultrasound may not be needed unless there is a high risk of uterine cancer.
- Women With Irregular Bleeding or Spotting
- A transvaginal ultrasound should be done to check the thickness of the endometrium.
- If the lining is thickened, an endometrial biopsy may be needed.
- Women With a History of Endometrial Hyperplasia
- More frequent ultrasounds and biopsies may be required.
- Some women may need to stop TT or adjust hormone therapy.
- Women on Long-Term Testosterone Therapy
- Regular check-ups with an endocrinologist or gynecologist are important.
- If there are no symptoms, an ultrasound may be done every few years, depending on individual risk factors.
Key Signs That Require Immediate Medical Attention
Women on TT should be aware of symptoms that could signal a problem with the uterus. If any of the following symptoms occur, a doctor should be consulted right away:
- Unusual vaginal bleeding, especially after menopause.
- Pelvic pain or pressure.
- A feeling of fullness or bloating in the lower abdomen.
- Unexplained weight loss.
- Changes in urination or bowel habits (if the uterus presses on nearby organs).
The Role of Doctors in Monitoring Women on Testosterone Therapy
Doctors play an important role in ensuring TT is safe and effective. Women on TT should work closely with their healthcare providers to:
- Monitor hormone levels regularly.
- Adjust TT if hormone imbalances are detected.
- Receive appropriate cancer screenings based on their medical history.
- Discuss any symptoms or concerns about TT’s effects on the uterus.
Testosterone therapy is an important treatment for many women, but it must be used with care. Because hormones play a key role in uterine health, special cancer screenings may be needed for women on TT. Regular check-ups, ultrasounds, and biopsies can help detect any problems early. Women should always discuss screening options with their doctors to ensure their health is monitored properly.
Conclusion: Weighing the Risks and Benefits of Testosterone Therapy in Uterine Cancer
Testosterone therapy (TT) is an important treatment option for many women, particularly those with low testosterone levels due to menopause, medical conditions, or gender-affirming care. However, concerns about its potential link to uterine cancer have led to debates in the medical community. While some researchers believe TT may increase the risk of uterine cancer, others suggest it could have protective effects. Because of the mixed findings, women considering TT must understand the risks and benefits before making a decision.
One of the key factors in this debate is the way testosterone interacts with other hormones in the body, especially estrogen and progesterone. The uterus is highly sensitive to hormonal changes, and both estrogen and progesterone play a role in endometrial health. When estrogen levels are too high without enough progesterone to balance them, the lining of the uterus (endometrium) may grow too much. This overgrowth, called endometrial hyperplasia, can increase the risk of uterine cancer.
Testosterone itself does not directly stimulate the uterine lining like estrogen does. However, in some cases, testosterone can convert into estrogen through a process called aromatization. This conversion depends on several factors, including the amount of testosterone taken, a woman’s body fat percentage, and how her body metabolizes hormones. If too much testosterone converts to estrogen, it could, in theory, increase the risk of endometrial hyperplasia and cancer.
On the other hand, some research suggests that testosterone may help counteract estrogen’s effects on the uterus. Studies have shown that testosterone can reduce endometrial growth and even lead to endometrial atrophy (thinning of the uterine lining). This effect could help lower the risk of cancer, especially in postmenopausal women or those with conditions like polycystic ovary syndrome (PCOS), where estrogen levels are often high. However, more research is needed to confirm whether testosterone truly offers protective benefits.
Women with a history of uterine cancer or those who are at high risk must be especially cautious when considering TT. Cancer survivors often have unique hormonal needs, and adding testosterone to the mix could have unexpected effects. Some studies suggest that TT does not increase the risk of uterine cancer recurrence, but there is still not enough data to say this with certainty. Because of this, women with a history of uterine cancer should work closely with their doctors to weigh the potential benefits of TT against the risks.
Another important concern is the impact of testosterone on endometrial thickness. Doctors use ultrasound to measure the thickness of the uterine lining because thicker linings can sometimes be a sign of cancer risk. Some studies suggest that TT may keep the endometrial lining thin, while others indicate that it could lead to irregular growth in certain women. This uncertainty makes regular monitoring essential for anyone using TT.
Another challenge is that TT can sometimes cause symptoms that overlap with signs of uterine cancer. Abnormal vaginal bleeding, pelvic pain, and weight changes are all symptoms of uterine cancer, but they can also occur as side effects of TT. This overlap can make it difficult to know whether symptoms are harmless or a sign of something more serious. Because of this, women on TT should report any unusual symptoms to their doctors and undergo appropriate testing when needed.
Due to the complex relationship between testosterone and the uterus, doctors may recommend additional cancer screenings for women on TT. Regular pelvic exams, transvaginal ultrasounds, and biopsies may be needed to monitor for any concerning changes in the uterine lining. Women using TT should also work with their healthcare providers to ensure their hormone levels are properly balanced. In some cases, combining TT with progesterone or other medications may help reduce risks.
In conclusion, the relationship between testosterone therapy and uterine cancer is still not fully understood. Some evidence suggests that TT could contribute to cancer risk by increasing estrogen levels, while other studies indicate it may help prevent uterine cancer by reducing endometrial growth. Because of these conflicting findings, more research is needed to determine the true impact of TT on the uterus.
For now, the best approach is to make individualized treatment decisions based on a woman’s unique health needs and risk factors. Women considering TT should have open discussions with their healthcare providers, undergo regular monitoring, and report any unusual symptoms as soon as they arise. By taking a cautious and well-informed approach, women can balance the benefits of testosterone therapy with their overall health and well-being.
Questions and Answers
The relationship between testosterone therapy and uterine cancer is not fully understood. Some studies suggest that high levels of androgens may contribute to endometrial hyperplasia, a precursor to uterine cancer, while others indicate that testosterone may have a protective effect by suppressing estrogen-driven endometrial growth.
Yes, testosterone therapy can lead to an imbalance between androgens and estrogens, potentially resulting in endometrial hyperplasia, which is a risk factor for uterine cancer.
Testosterone can be converted into estrogen through aromatization, which may stimulate endometrial growth. However, in some cases, testosterone therapy may also lead to endometrial atrophy, reducing the risk of hyperplasia.
Generally, individuals with a history of uterine cancer should consult their doctor before starting testosterone therapy. Some healthcare providers may recommend alternative treatments or additional monitoring.
Some research suggests that testosterone may suppress estrogen-induced endometrial growth, which could lower the risk of uterine cancer. However, more studies are needed to confirm this effect.
Patients undergoing testosterone therapy should have regular gynecological exams, including ultrasounds and endometrial biopsies if necessary, to monitor changes in the uterine lining.
There is limited research on this topic, but current evidence does not strongly suggest that testosterone therapy significantly increases uterine cancer risk in transgender men. However, ongoing monitoring is recommended.
Symptoms include abnormal vaginal bleeding, pelvic pain, and unusual discharge. Any persistent changes should be evaluated by a healthcare provider.
Yes, progesterone can help counteract estrogen’s effects on the endometrium, potentially reducing the risk of endometrial hyperplasia and cancer in individuals receiving testosterone therapy.
They should seek medical evaluation immediately to rule out endometrial hyperplasia or cancer. A doctor may recommend an ultrasound or biopsy to assess the condition of the uterine lining.