Introduction
Luteinizing hormone (LH) is a pivotal hormone in human biology, with far-reaching effects on both reproductive health and general well-being. This article aims to unravel the complexities of LH, offering a comprehensive exploration of its functions, importance, and impact on health. Our journey into the world of LH will traverse its chemical nature, its crucial roles in both male and female reproductive systems, and its broader implications on overall health.
LH, produced by the anterior pituitary gland, is not just a singular entity in the hormonal orchestra but a key conductor. Its levels and activities are delicately balanced in a symphony of biochemical signals and responses. Understanding LH is not merely about comprehending a hormone; it's about decoding a fundamental aspect of human physiology that influences myriad health aspects – from fertility to hormonal balance, and from puberty to aging.
This hormone's relevance transcends gender, playing integral roles in both males and females. In women, LH is a central player in the menstrual cycle and ovulation, directly impacting fertility. In men, it drives testosterone production, influencing everything from muscle mass to mood. The LH surge, a critical phenomenon in the female reproductive cycle, is a focal point of understanding female fertility and reproductive health.
The significance of LH extends into various medical realms. Its levels are pivotal in diagnosing and treating reproductive and endocrine disorders. Disturbances in LH production or function can lead to conditions like polycystic ovary syndrome (PCOS), infertility, and pituitary disorders, making it a crucial marker in reproductive health diagnostics.
As we delve into this article, each section will shed light on different aspects of LH. We will explore its roles, its impact on health, the conditions associated with its imbalance, and the latest research trends. This comprehensive guide aims to answer the most pressing questions about LH, informed by the latest scientific research and expert insights. Join us in decoding the mysteries of luteinizing hormone and understanding its paramount role in health and disease.
Understanding Luteinizing Hormone
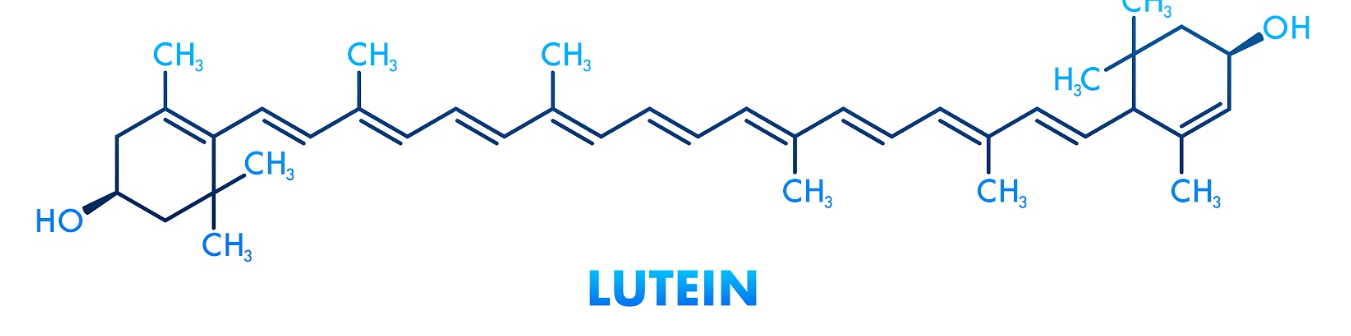
Luteinizing Hormone (LH) is a crucial component in the intricate machinery of the human endocrine system. This glycoprotein hormone, synthesized and secreted by the anterior pituitary gland, plays a pivotal role in regulating reproductive processes in both men and women. To fully appreciate the significance of LH, it's essential to understand its biochemical nature, production mechanisms, and regulatory pathways.
At its core, LH is a glycoprotein composed of two subunits, alpha and beta, which are intertwined to form its active structure. The alpha subunit is similar to that of other hormones like follicle-stimulating hormone (FSH), thyroid-stimulating hormone (TSH), and human chorionic gonadotropin (hCG), while the beta subunit is unique to LH, conferring its specific biological action.
LH production is regulated by a complex interplay of signals within the hypothalamic-pituitary-gonadal axis. The hypothalamus, a critical brain region, secretes Gonadotropin-releasing hormone (GnRH) in a pulsatile manner, which in turn stimulates the anterior pituitary gland to release LH into the bloodstream. This pulsatile release is crucial for the proper functioning of LH, as continuous exposure to GnRH can lead to decreased responsiveness of the pituitary gland.
Once released, LH acts on the gonads – the ovaries in females and the testes in males. In females, LH triggers ovulation and stimulates the corpus luteum to produce progesterone, a hormone vital for maintaining pregnancy. In males, LH stimulates the Leydig cells in the testes to produce testosterone, which is essential for spermatogenesis and the development of male secondary sexual characteristics.
The regulation of LH is a fine balance, primarily achieved through a feedback loop involving sex steroids like estrogen and testosterone. Elevated levels of these steroids typically signal the pituitary gland to reduce LH production, while low levels prompt an increase in LH secretion. This feedback mechanism ensures the maintenance of hormonal balance and proper functioning of the reproductive system.
Furthermore, factors such as stress, physical activity, and certain medical conditions can influence LH levels, underscoring the hormone's sensitivity to both internal and external environments. Understanding LH's production and regulation is therefore not only a window into the workings of the reproductive system but also an insight into how various factors can impact our overall endocrine health.
The Role of LH in the Reproductive System
Luteinizing Hormone (LH) plays a fundamental and multifaceted role in the human reproductive system. Its importance spans both male and female physiology, underpinning key reproductive processes. In this section, we delve into the specific functions of LH, highlighting its critical roles and the consequences of its imbalance in reproductive health.
In women, LH is instrumental in orchestrating the menstrual cycle. It works in tandem with Follicle-Stimulating Hormone (FSH), another pituitary hormone, in a delicate dance of hormonal interplay. Early in the menstrual cycle, LH supports the development of ovarian follicles, the structures that contain and nurture the developing eggs. As the cycle progresses, rising estrogen levels from the maturing follicles trigger a surge in LH production. This LH surge is a defining moment in the menstrual cycle, culminating in the rupture of the dominant follicle and the release of an egg — a process known as ovulation. Post-ovulation, LH helps transform the remnants of the ruptured follicle into the corpus luteum, which secretes progesterone to prepare the uterus for potential pregnancy.
For men, LH's role is centered on testosterone production. It stimulates the Leydig cells in the testes to produce testosterone, a hormone pivotal not only for the development of male secondary sexual characteristics but also crucial for spermatogenesis, the process of sperm production. Testosterone's influence extends beyond the reproductive system, impacting muscle mass, bone density, and even mood.
The significance of LH in both sexes underscores its vital role in overall reproductive health. Imbalances in LH levels can lead to a host of reproductive issues. In women, abnormal LH levels are often implicated in conditions like polycystic ovary syndrome (PCOS) and anovulation, both of which can lead to infertility. In men, low LH levels can result in decreased testosterone production, affecting fertility, sexual function, and overall health.
Understanding LH's role in the reproductive system is not just about comprehending a biological process; it's about recognizing a key element in human health and well-being. This hormone's influence spans from the molecular level to the systemic, affecting not just individual health but also the reproductive potential of the population. As we continue to explore LH's multifaceted roles, it becomes evident that this hormone is more than just a cog in the reproductive machinery; it's a critical component in the complex tapestry of human biology.
LH and the Menstrual Cycle
The role of Luteinizing Hormone (LH) in the menstrual cycle is pivotal, marking its significance as a key regulator of female reproductive health. The menstrual cycle, a complex interplay of hormones and physiological processes, relies heavily on the precise and timely actions of LH to facilitate its various phases, most notably ovulation.
In the early stages of the menstrual cycle, LH works subtly yet significantly alongside Follicle-Stimulating Hormone (FSH). Together, they stimulate the growth and maturation of ovarian follicles, each containing a potential ovum. LH's role in this phase is more of a supporting act, helping to prepare the follicles for the imminent surge that will trigger ovulation.
As the cycle progresses, estrogen levels, primarily from the maturing follicles, begin to rise. This increase in estrogen creates a feedback loop to the pituitary gland and hypothalamus. When estrogen reaches a threshold level, it triggers a dramatic and crucial event in the menstrual cycle: the LH surge. This surge is a rapid and significant increase in LH levels, occurring approximately in the middle of the menstrual cycle.
The LH surge is the key that unlocks ovulation. It causes the mature follicle to release its ovum, marking the transition from the follicular phase to the luteal phase of the menstrual cycle. Post-ovulation, the role of LH shifts. It aids in transforming the remnants of the ruptured follicle into the corpus luteum, a temporary endocrine structure. The corpus luteum, under LH's influence, produces progesterone, a hormone critical for preparing the uterus for a potential pregnancy.
Should fertilization not occur, the corpus luteum degenerates, leading to a drop in progesterone levels. This decrease signals the shedding of the uterine lining, known as menstruation, and the commencement of a new menstrual cycle.
Understanding LH's role in the menstrual cycle reveals not only its importance in ovulation but also its broader impact on female reproductive health. Abnormalities in LH secretion can disrupt the menstrual cycle, leading to issues such as irregular periods, anovulation, or infertility. Thus, LH is not just a hormone that acts at a specific stage; it is a crucial orchestrator of the entire menstrual cycle, influencing a woman's reproductive health and fertility.
LH in Males: Testosterone Production and More
Luteinizing Hormone (LH) serves a pivotal role in male physiology, particularly in the realm of reproductive health and hormonal balance. While often associated with female reproductive processes, LH's influence in males is equally crucial, primarily orchestrating testosterone production and influencing various aspects of male health.
In the male body, LH is produced by the anterior pituitary gland and functions as a key stimulator of testosterone synthesis. Its primary target is the Leydig cells in the testes. Upon LH's binding to its receptors on these cells, a cascade of biochemical events ensues, leading to the synthesis and release of testosterone. This hormone, central to male reproductive health, is responsible for the development of male secondary sexual characteristics, such as increased muscle mass, deeper voice, and body hair. Moreover, testosterone plays a significant role in spermatogenesis – the production of sperm – highlighting LH's indirect but vital contribution to male fertility.
The relationship between LH and testosterone is governed by a feedback mechanism crucial for maintaining hormonal balance. Elevated testosterone levels signal the hypothalamus and pituitary gland to reduce the production of LH, while low testosterone levels prompt an increase in LH secretion. This feedback loop ensures the maintenance of optimal testosterone levels, which is essential for overall health, well-being, and reproductive function.
LH's role in men extends beyond testosterone production. It is intricately linked with general health parameters such as bone density, muscle strength, and even mood and libido. Abnormal levels of LH can lead to various health challenges. Low LH levels, for instance, may result in hypogonadism – a condition characterized by insufficient testosterone production. This can manifest in reduced libido, erectile dysfunction, decreased muscle mass, and a range of other health issues. Conversely, high LH levels could indicate underlying problems such as testicular failure or pituitary disorders.
Understanding the role of LH in male health is essential not only for addressing specific reproductive disorders but also for appreciating its broader impact on male health and well-being. Regular health assessments, including hormone level checks, are key to detecting and addressing any imbalances early on. LH, therefore, is not just a reproductive hormone but a crucial marker of male health, underscoring the complex interplay between hormones and overall physiological functioning.
Health Conditions Associated with LH Imbalance
Luteinizing Hormone (LH) plays a critical role in regulating reproductive functions in both men and women. However, imbalances in LH levels can lead to a variety of health conditions, underscoring the hormone's significance beyond its primary reproductive role. Understanding the conditions associated with LH imbalance is crucial for diagnosing and managing various reproductive and hormonal disorders.
In women, one of the most common conditions linked to abnormal LH levels is Polycystic Ovary Syndrome (PCOS). Characterized by hormonal imbalance and metabolic issues, PCOS often involves elevated LH levels, which can disrupt the normal functioning of the ovaries, leading to irregular menstrual cycles, difficulties with ovulation, and challenges in conceiving. Women with PCOS may also experience symptoms such as weight gain, acne, and excessive hair growth due to the hormonal imbalances.
Another condition related to LH imbalance in women is primary ovarian insufficiency (POI), where the ovaries cease to function properly before the age of 40. This can result in high LH levels as the pituitary gland tries to stimulate the non-responsive ovaries. POI can lead to infertility, early menopause symptoms, and increased risk of osteoporosis.
In men, imbalances in LH levels can result in conditions affecting fertility and overall health. Low LH levels can lead to hypogonadism, where the body produces insufficient testosterone. Symptoms of hypogonadism include reduced libido, erectile dysfunction, decreased muscle mass, and fatigue. In contrast, high LH levels in men can indicate testicular failure or damage, which can also impact fertility and testosterone production.
LH imbalances can also signify broader endocrine disorders, such as pituitary gland disorders. The pituitary gland, which produces LH, can be affected by tumors, congenital conditions, or injury, leading to either overproduction or underproduction of LH and other hormones.
Diagnosing and treating conditions related to LH imbalance require a comprehensive approach, including hormonal assessments, medical history evaluation, and, in some cases, genetic testing. Understanding these conditions is not only crucial for reproductive health but also for overall well-being, as hormonal imbalances can affect various aspects of physical and mental health. Therefore, LH serves as a vital marker in diagnosing and managing a range of health conditions, reflecting the intricate relationship between hormones and bodily functions.
Diagnostic and Therapeutic Uses of LH Testing
The measurement of Luteinizing Hormone (LH) levels plays a crucial role in diagnosing and treating various reproductive and hormonal disorders. LH testing is a key tool in the medical field, aiding in the understanding and management of conditions related to reproductive health and endocrine function. This section explores the diagnostic and therapeutic applications of LH testing in clinical settings.
Diagnostic Uses: LH testing is instrumental in evaluating reproductive health in both men and women. In women, it is commonly used to assess ovulatory function and menstrual irregularities. For instance, LH tests can help diagnose conditions like Polycystic Ovary Syndrome (PCOS) and primary ovarian insufficiency, both of which involve altered LH levels. Additionally, measuring LH surge is crucial for determining the timing of ovulation, an essential factor for couples trying to conceive.
In men, LH testing is significant for evaluating testicular function and diagnosing conditions such as hypogonadism. Abnormal LH levels can indicate underlying issues with the testes or hormonal regulation, affecting testosterone production and fertility. LH tests can also aid in diagnosing pituitary disorders that affect LH production, thus impacting reproductive function.
Therapeutic Uses: Beyond diagnostics, LH testing has therapeutic applications, particularly in fertility treatments. In assisted reproductive technologies like in vitro fertilization (IVF), monitoring LH levels is crucial for timing egg retrieval and optimizing the chances of successful fertilization. LH tests also guide hormone replacement therapy, both in men and women, by helping to adjust dosages to achieve the desired hormonal balance.
For individuals with infertility issues related to LH imbalance, LH testing is vital for developing effective treatment plans. For example, women with anovulation may receive treatments that stimulate the LH surge to induce ovulation. In men with low testosterone due to insufficient LH production, hormone therapy can be adjusted based on LH test results to improve fertility and overall health.
The role of LH testing in the medical field is multifaceted, encompassing both diagnostic and therapeutic realms. Its ability to provide insights into hormonal balance and reproductive function makes it an invaluable tool in modern medicine. Understanding the significance of LH in various health conditions is essential for clinicians and patients alike, as it informs treatment decisions and improves patient outcomes. Therefore, LH testing is more than just a measure of a single hormone; it is a window into the complex interplay of the endocrine system and its impact on human health.
Lifestyle and LH: The Impact of Diet and Exercise
The influence of lifestyle factors, particularly diet and exercise, on Luteinizing Hormone (LH) levels and overall reproductive health is profound. Lifestyle choices can significantly affect hormonal balance, emphasizing the importance of a holistic approach to maintaining reproductive health. In this section, we explore how diet and exercise impact LH levels and the potential consequences on reproductive function.
Diet and LH Levels: Nutrition plays a crucial role in regulating hormonal balance, including LH levels. Certain nutrients and dietary patterns can influence the production and function of LH. For instance, diets rich in polyunsaturated fatty acids (PUFAs) have been shown to affect LH secretion positively. On the other hand, excessive intake of refined sugars and processed foods can disrupt hormonal balance, potentially leading to irregularities in LH levels.
Research also suggests that diets with adequate protein, healthy fats, and essential vitamins and minerals support the endocrine system's optimal function. For example, zinc, found in nuts, seeds, and lean meats, is crucial for hormone production, including LH. Similarly, vitamin D, obtained from sunlight exposure and certain foods, has been linked to healthy LH levels.
Exercise and LH Levels: Physical activity exerts a significant impact on hormonal health. Moderate exercise has been shown to improve LH secretion and overall hormonal balance. Regular physical activity can enhance reproductive health by improving body composition, reducing stress, and enhancing metabolic function, all of which can positively influence LH levels.
However, it's important to note that excessive exercise, particularly in females, can lead to disruptions in LH secretion. Overtraining and high-intensity exercise regimens can result in decreased LH levels, leading to menstrual irregularities and fertility issues, a condition often seen in athletes known as the 'female athlete triad.'
The interaction between lifestyle factors and LH levels highlights the importance of a balanced approach to diet and exercise for maintaining hormonal health. Adopting a diet rich in essential nutrients and engaging in regular, moderate physical activity can support healthy LH levels, thereby promoting optimal reproductive health. This connection underscores the integral relationship between lifestyle choices and hormonal balance, advocating for a comprehensive approach to health and well-being.
LH Research: Current Trends and Future Directions
The field of Luteinizing Hormone (LH) research is continuously evolving, with new studies shedding light on its multifaceted roles and potential therapeutic applications. This expanding body of research not only enhances our understanding of LH in reproductive health but also explores its implications in broader physiological and pathological contexts. In this section, we delve into the current trends in LH research and look ahead at the promising directions this research might take.
Recent Trends in LH Research: Current research on LH is focusing on unraveling its complex interactions within the endocrine system and its broader impact on health. Studies are examining the molecular mechanisms of LH action, aiming to better understand how LH influences cellular processes in the gonads and beyond. There's a growing interest in how LH interacts with other hormones and how these interactions can be modulated for therapeutic benefits.
Another area of active research is the role of LH in conditions like polycystic ovary syndrome (PCOS) and infertility. Scientists are exploring how LH levels affect the development of these conditions and how altering LH activity can lead to new treatment strategies. This research is particularly crucial, as it could provide more effective and targeted therapies for individuals struggling with reproductive health issues.
Future Directions in LH Research: Looking forward, LH research is poised to delve deeper into the hormone's role in non-reproductive aspects of health. This includes investigating its potential influences on metabolic processes, aging, and even mental health. Understanding these relationships could open new avenues for treating a range of conditions that have hormonal components.
Additionally, advancements in biotechnology and genetic engineering are paving the way for more sophisticated studies on LH. This includes developing novel LH analogs or inhibitors that can be used in clinical settings for treating hormonal imbalances or reproductive disorders. Personalized medicine approaches, which consider individual hormonal profiles, could also benefit from deeper insights into LH function.
The future of LH research holds great promise for improving human health. By continuing to explore the hormone's complex roles and interactions, scientists can develop more effective treatments for a range of conditions and enhance our overall understanding of human physiology. This ongoing research is not just about LH in isolation but about integrating this knowledge into a broader context of endocrine function and health.
Conclusion
As we conclude our in-depth exploration of Luteinizing Hormone (LH), it's evident that this hormone plays a crucial role far beyond its basic functions in the reproductive system. The journey through the various facets of LH has illuminated its significance in both male and female health, its intricate regulatory mechanisms, and its impact on various health conditions. This comprehensive overview underscores the complexity and importance of LH in human physiology.
In women, LH's role in the menstrual cycle, particularly in triggering ovulation, is vital for fertility and reproductive health. Its imbalance can lead to conditions like polycystic ovary syndrome (PCOS) and infertility, highlighting the importance of maintaining hormonal balance. In men, LH's influence on testosterone production underscores its importance in male reproductive health and overall well-being. Imbalances in LH can result in conditions such as hypogonadism, affecting not only fertility but also other aspects of health like bone density and muscle mass.
The diagnostic and therapeutic applications of LH testing have shown us how crucial this hormone is in the clinical setting. From guiding fertility treatments to helping diagnose reproductive and endocrine disorders, LH testing is an invaluable tool in modern medicine. The intersection of lifestyle factors like diet and exercise with LH levels further illustrates how our daily choices impact our hormonal health.
Looking at the current trends and future directions of LH research, it's clear that there's still much to uncover about this hormone's roles and impacts. The ongoing research is expanding our understanding of LH's functions and its potential applications in treating a range of conditions, both reproductive and beyond.
In summary, LH is not just a hormone; it's a key player in the complex symphony of human biology. Its influence extends from the cellular level to the whole body, affecting not just reproductive health but also general well-being. As we continue to learn more about LH and its myriad roles, we gain deeper insights into the intricate workings of the human body and the delicate balance of our endocrine system.
In this section, we address the top questions related to Luteinizing Hormone (LH), providing insightful answers based on current scientific understanding. These questions encompass a range of topics concerning LH's functions, importance, and impact on health, reflecting common inquiries from individuals seeking to understand this crucial hormone.
By addressing these questions, we aim to provide a comprehensive understanding of LH, its functions, and its significance in human health. This knowledge not only offers insights into reproductive health but also underscores the hormone's broader impact on overall well-being.