Does Testosterone Therapy Affect Cholesterol Levels? A Complete Evidence-Based Guide
Introduction
Testosterone therapy, also called testosterone replacement therapy (TRT), is one of the most talked about medical treatments today. It is often prescribed to men who have very low testosterone levels, a condition known as hypogonadism. Some men may also receive it for age-related decline in testosterone or for certain medical conditions when a doctor believes it can improve quality of life. Over the past two decades, prescriptions for testosterone therapy have greatly increased. More people are asking whether this therapy has risks for the heart and blood vessels, especially because cholesterol levels are one of the strongest predictors of heart disease.
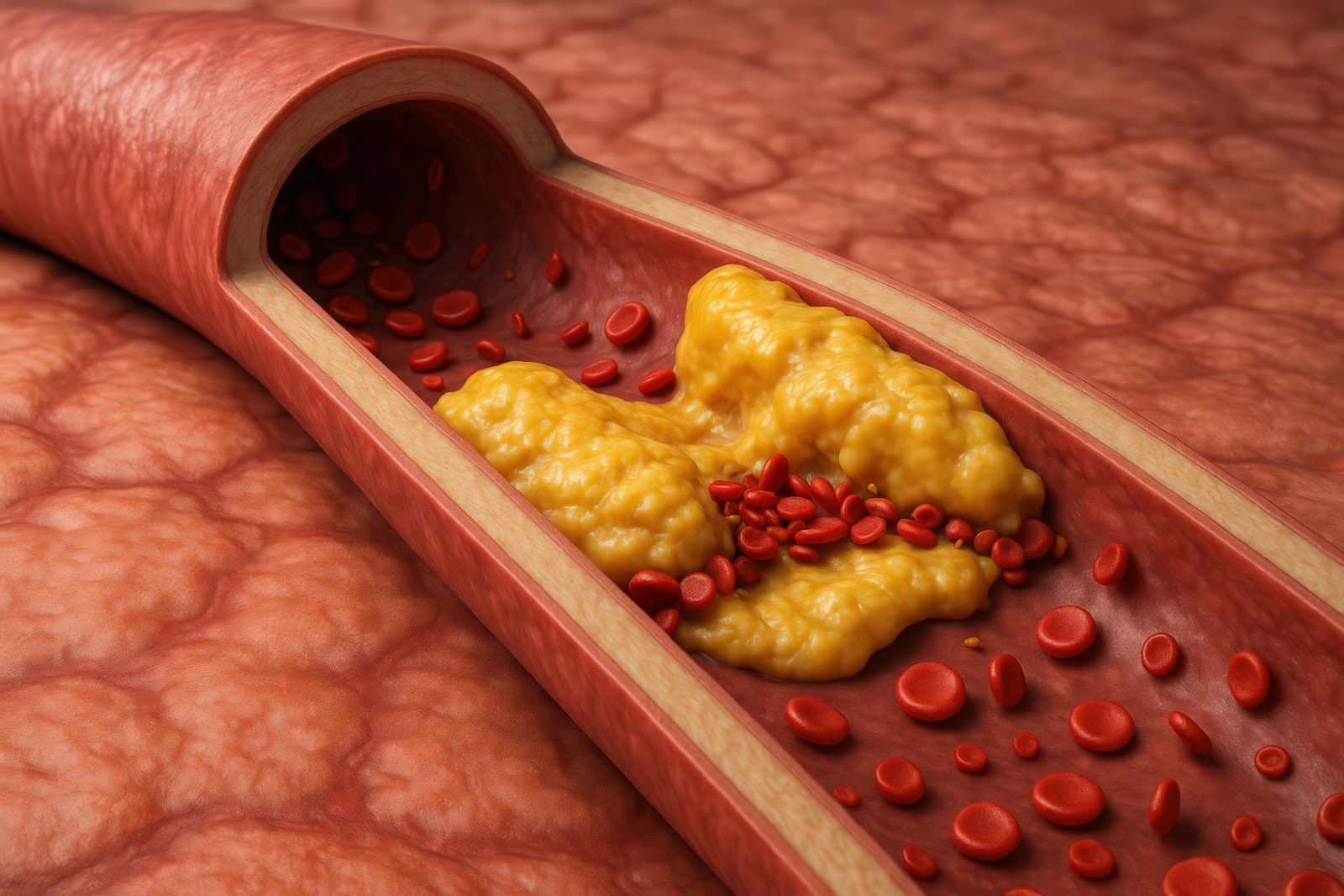
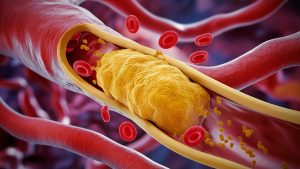
Cholesterol itself is not a bad thing. It is a type of fat that the body needs for building hormones, vitamin D, and cell membranes. But when cholesterol levels are not balanced, problems can occur. There are different types of cholesterol. Low-density lipoprotein cholesterol (LDL) is often called “bad cholesterol” because high levels can lead to a build-up of fatty plaques in arteries. High-density lipoprotein cholesterol (HDL) is often called “good cholesterol” because it helps clear LDL from the bloodstream. Triglycerides are another kind of fat in the blood, and high levels of these can also raise the risk of heart disease. Because cholesterol and triglycerides are so closely tied to heart health, doctors pay very close attention to how different medicines, including testosterone therapy, affect these blood fats.
The relationship between testosterone and cholesterol is not simple. Testosterone is a natural hormone that the body makes mainly in the testicles in men, and in smaller amounts in women’s ovaries and adrenal glands. It plays a key role in sexual health, energy, muscle strength, bone density, and mood. When levels of testosterone are too low, men may experience symptoms such as fatigue, weight gain, depression, or a drop in sexual function. Giving testosterone in the form of injections, gels, patches, or pellets can often improve these symptoms. But hormones affect many systems in the body, and the way testosterone interacts with cholesterol is still being studied.
Some research shows that testosterone therapy can lower HDL, the “good” cholesterol, which may not be ideal because HDL helps protect the heart. Other studies suggest it might raise LDL or have little effect on it. Still other studies find improvements in triglycerides or no significant changes at all. These mixed results make it hard for patients and even doctors to know exactly what to expect. The type of testosterone treatment, the dose, the length of therapy, and the health of the patient before starting all seem to influence the outcome.
Another reason this topic matters is because heart disease is the number one cause of death worldwide. Anything that changes cholesterol levels can, in theory, change a person’s risk of having a heart attack or stroke. Many men who consider testosterone therapy are already older, and some may already have risk factors like obesity, high blood pressure, or diabetes. For these men, the effects of testosterone on cholesterol are especially important.
This article provides a clear and complete evidence-based guide to answer the most common questions people search about testosterone therapy and cholesterol. It will explore whether testosterone raises or lowers cholesterol, how it affects LDL, HDL, and triglycerides, whether the type of therapy matters, and what all this means for long-term heart health. It will also discuss how age, medical conditions, and lifestyle factors like diet and exercise interact with testosterone’s effects. Finally, it will explain how often cholesterol should be checked while someone is on testosterone therapy and what both patients and doctors need to know when deciding on treatment.
By the end of this guide, you will understand what science currently says about testosterone therapy and cholesterol. While there are still debates in the medical community, we will carefully review the latest research in a way that is easy to follow. This is not a collection of personal stories or opinions, but a structured look at what clinical studies, expert reviews, and guidelines have found. Since health decisions should always be made with good information, this guide aims to make a complex subject clear and practical.
In short, testosterone therapy is more than just a treatment for low energy or poor sexual health. It is a hormone therapy that can change many systems in the body. Because cholesterol levels are closely tied to the health of the heart and blood vessels, understanding the link between testosterone therapy and cholesterol is one of the most important questions for anyone considering or already using this treatment. This introduction sets the stage for the deeper dive ahead, where each of the top questions will be answered in detail, using the best available evidence.
What Is Testosterone Therapy and Why Is It Prescribed?
Testosterone therapy, often called TRT (testosterone replacement therapy), is a medical treatment designed to restore testosterone levels in people whose bodies do not make enough of this hormone on their own. Testosterone is one of the main male sex hormones, though it is present in both men and women. It plays a central role in energy levels, sexual health, muscle and bone strength, red blood cell production, and overall sense of well-being.
When the body does not produce enough testosterone, a condition called hypogonadism, symptoms such as low energy, reduced sexual desire, erectile difficulties, muscle weakness, loss of bone density, mood changes, and even memory problems can appear. In these cases, doctors may recommend testosterone therapy to bring hormone levels back to a healthy range.
FDA-Approved Uses of Testosterone Therapy
In the United States, the Food and Drug Administration (FDA) has approved testosterone therapy for very specific medical conditions. These include:
- Primary hypogonadism – This happens when the testes cannot make enough testosterone due to injury, infection, or a genetic problem.
- Secondary hypogonadism – This occurs when the pituitary gland or hypothalamus in the brain fails to signal the testes to produce testosterone. Causes can include pituitary tumors, certain brain injuries, or chronic illness.
For these conditions, testosterone therapy is considered a standard and accepted treatment because the hormone levels are truly low due to medical disease.
Off-Label Uses and Age-Related Decline
In addition to the approved uses, some doctors prescribe testosterone therapy for men whose testosterone levels naturally fall with age. Starting around age 30, testosterone begins to decline by about 1% per year. This can lead to symptoms such as tiredness, loss of strength, weight gain, and sexual difficulties.
Prescribing testosterone therapy in this context is called off-label use, because the FDA has not formally approved testosterone for normal aging. Still, many men seek TRT in hopes of reversing some of these age-related changes. This practice is growing, but it also comes with controversy. Medical experts continue to study whether testosterone therapy is safe and effective for older men who do not have a clear medical disorder.
Different Forms of Testosterone Therapy
Doctors can prescribe testosterone in several different forms. Each has its own benefits, drawbacks, and effects on cholesterol and heart health. The most common types include:
- Injections: Testosterone is often injected into the muscle every 1–4 weeks. Some long-acting injections can last longer. Injections can cause hormone levels to rise and fall sharply, which some patients feel as mood or energy swings.
- Gels: These are applied daily to the skin, usually on the shoulders, arms, or abdomen. The gel slowly releases testosterone into the bloodstream. A major concern is accidental transfer to another person through skin contact.
- Patches: Worn on the skin, patches deliver testosterone steadily. They can sometimes cause skin irritation.
- Pellets: Small pellets are implanted under the skin by a doctor. They release testosterone gradually over several months. This option avoids daily treatment but requires a minor surgical procedure.
- Oral capsules or tablets: These exist but are less commonly prescribed in the U.S. because they can affect the liver. Newer oral formulations are being studied for safety.
The choice of therapy often depends on the patient’s lifestyle, medical history, cost, and personal preference.
General Benefits of Testosterone Therapy
When used appropriately, testosterone therapy can help restore quality of life for men with low testosterone. Documented benefits may include:
- Energy and mood: Many men report feeling less tired and more motivated. Some also experience reduced irritability and depression.
- Sexual health: TRT can improve libido (sex drive) and help with erectile function in men with hormone-related sexual problems.
- Muscle mass and strength: Testosterone plays a major role in building and maintaining muscle tissue. Replacement therapy can reverse muscle loss and improve physical strength.
- Bone density: Low testosterone is linked to osteoporosis (weak bones). TRT may increase bone density and reduce fracture risk.
- Red blood cell production: Testosterone stimulates the bone marrow to make more red blood cells, which can improve oxygen delivery and stamina. However, this also raises the risk of thickened blood, so monitoring is needed.
It is important to note that these benefits are best documented in men who truly have low testosterone due to medical causes. The benefits in otherwise healthy older men with only mildly low levels remain less certain.
Testosterone therapy is a treatment meant to restore normal hormone levels in people with a proven deficiency. While the FDA approves it for men with medical hypogonadism, many men also receive it for age-related decline, even though this use is not officially approved. TRT can be delivered in several forms, such as injections, gels, patches, or pellets, and each method has unique advantages and risks.
The therapy aims to improve energy, sexual health, muscle and bone strength, and overall well-being. At the same time, it requires medical supervision because of possible side effects, including changes in cholesterol levels and heart health, which will be explored in later sections of this article.
How Does Testosterone Affect Cholesterol in the Body?
To understand how testosterone therapy may change cholesterol levels, we first need to look at how cholesterol works in the body and what role testosterone plays in regulating it. Cholesterol is not always “bad.” In fact, your body needs cholesterol to build hormones, vitamin D, and healthy cell walls. But cholesterol is carried in the blood by different particles, and the balance between these particles determines heart health. Testosterone, being a sex hormone, influences many parts of metabolism, including how the body processes cholesterol and fats.
In this section, we will explore the basic science behind testosterone and cholesterol, the biological pathways involved, and the difference between natural testosterone and therapy using external sources (called exogenous testosterone).
Testosterone’s Role in Lipid Metabolism
Lipids are fats, and cholesterol is one type of lipid. Testosterone affects lipid metabolism, which means how the body makes, uses, and clears fats from the blood. Studies show that testosterone can interact with the liver, the main organ that produces and manages cholesterol. The liver regulates two key types of cholesterol-carrying particles:
- LDL (Low-Density Lipoprotein): Often called “bad cholesterol,” because high levels can lead to plaque buildup in arteries.
- HDL (High-Density Lipoprotein): Known as “good cholesterol,” because it helps remove extra cholesterol from the bloodstream.
Testosterone appears to lower HDL levels in some people, while its effect on LDL is less consistent. Some men may see a small increase in LDL, while others notice little change. The way testosterone acts depends on many factors, such as age, dose, type of therapy, and individual metabolism.
Mechanisms: How Testosterone May Influence Cholesterol
Researchers have studied how testosterone interacts with enzymes and receptors in the body that control cholesterol balance. Some of the key mechanisms include:
- Hepatic Lipase Activity:
Testosterone increases the activity of an enzyme called hepatic lipase. This enzyme helps break down HDL cholesterol. More hepatic lipase activity often means lower HDL levels in the blood. This is one of the most consistent findings about testosterone’s effect on cholesterol. - LDL Receptors:
Testosterone may reduce the number of LDL receptors in the liver. These receptors help remove LDL from the blood. If there are fewer receptors, LDL may rise. However, the evidence here is mixed, and not every study shows the same result. - Triglyceride Handling:
Testosterone may improve how muscles and fat cells use triglycerides, which are another type of blood fat. In some studies, this leads to lower triglyceride levels, especially in men who are overweight or have insulin resistance. - Body Composition Effects:
Testosterone therapy can reduce fat mass and increase muscle mass. Since excess body fat is linked to worse cholesterol levels, these changes may indirectly improve cholesterol. But this benefit might be partly offset by the drop in HDL.
Endogenous Testosterone vs. Exogenous Testosterone
It is important to separate natural (endogenous) testosterone from testosterone therapy (exogenous).
- Endogenous testosterone: This is the testosterone your body produces naturally. Men with higher natural testosterone levels often have healthier body composition (less fat, more muscle), which may support better cholesterol profiles. But even naturally high testosterone can sometimes mean lower HDL levels.
- Exogenous testosterone: This is testosterone introduced from outside the body, such as through injections, gels, or patches. Because therapy delivers higher or steadier doses than the body would naturally produce, the effects on cholesterol can be stronger. Exogenous testosterone has been more clearly linked to a decrease in HDL and potential changes in LDL.
Dose and Duration Matter
The amount and length of testosterone exposure can change cholesterol effects.
- Low to moderate doses used for medical treatment in men with low testosterone usually cause small changes in cholesterol.
- High doses (such as those sometimes misused by athletes for bodybuilding) can cause larger drops in HDL and may raise LDL, increasing heart risks.
- Short-term therapy may show mild or no changes, while long-term therapy can make patterns clearer, especially in middle-aged and older men.
Why These Changes Matter
Even small shifts in cholesterol caused by testosterone therapy may affect long-term heart health. A drop in HDL is especially concerning because HDL protects against plaque buildup in arteries. On the other hand, improvements in body fat, blood sugar control, and inflammation from testosterone therapy may reduce risks in other ways. This makes the overall picture complex.
Doctors weigh both the direct effects on cholesterol and the indirect benefits when deciding if testosterone therapy is safe for a patient. Regular blood testing helps track whether cholesterol changes are significant.
Testosterone influences cholesterol in several ways. It often lowers HDL, may slightly raise LDL, and sometimes improves triglyceride handling. These effects depend on whether the testosterone is natural or given as therapy, the dose and form used, and the person’s overall health. By understanding these mechanisms, patients and doctors can better predict what might happen during therapy and why close monitoring is important.
Does Testosterone Therapy Increase LDL ("Bad Cholesterol")?
One of the most common questions about testosterone therapy (TRT) is whether it raises levels of low-density lipoprotein (LDL) cholesterol, often called “bad cholesterol.” LDL matters because it can build up in the walls of blood vessels, creating plaques that narrow arteries and increase the risk of heart disease and stroke. Since heart health is a major concern for people considering TRT, understanding the research on this issue is important.
What Is LDL and Why Does It Matter?
LDL cholesterol carries fat molecules through the blood to tissues. While some LDL is necessary for normal body function, too much can harm blood vessels over time. High LDL is strongly linked to atherosclerosis, a condition in which plaques form inside arteries. These plaques can limit blood flow or break apart, leading to heart attack or stroke.
When patients ask if testosterone therapy “increases LDL,” they are really asking whether TRT makes the blood more likely to cause cardiovascular disease.
What the Research Shows About TRT and LDL
Clinical Trials
Many studies have looked at how testosterone therapy affects cholesterol levels, but results are not always the same. Some clinical trials show that LDL levels increase slightly in men receiving testosterone, while others find little to no change.
For example:
- Short-term trials (lasting 3–6 months) often report minimal changes in LDL.
- Longer-term studies (one year or more) sometimes show modest increases, especially with higher doses.
Overall, the evidence suggests that if LDL does rise, the change is usually small. Most studies report increases of less than 10 milligrams per deciliter (mg/dL), which may not be clinically significant for many patients.
Meta-Analyses
Meta-analyses, which combine data from many studies, provide a clearer picture. Several reviews have found that testosterone therapy tends to reduce total cholesterol and triglycerides slightly, but it may also lower protective HDL cholesterol. Changes in LDL are inconsistent: some analyses show a small rise, while others show no significant effect.
This mixed evidence means doctors cannot say with certainty that TRT universally raises LDL, but they remain cautious—especially for men with preexisting heart risks.
Role of Dosage and Delivery Method
The way testosterone is given may influence its effect on LDL cholesterol.
- Injectable testosterone: Some studies suggest that injections, especially high-dose regimens, are more likely to increase LDL compared with gels or patches. This may be because injections create higher peaks of testosterone in the blood.
- Transdermal testosterone (gels, creams, patches): These forms deliver steadier hormone levels and may have less impact on LDL.
- Oral testosterone: Rarely used in the United States because of liver side effects, oral forms have been associated with more pronounced changes in cholesterol, including higher LDL.
This means that not all patients experience the same cholesterol response. How testosterone is delivered matters.
Differences Between Short-Term and Long-Term Use
Time plays a role in how testosterone affects cholesterol.
- Short-term use (weeks to months): LDL levels often stay about the same or change only slightly.
- Long-term use (years): Some men may see gradual increases in LDL. However, lifestyle changes that often accompany TRT—such as improved energy leading to more exercise—can counteract this effect in some individuals.
Because of this, doctors usually recommend checking cholesterol levels regularly during therapy to catch any changes early.
Why the Effect on LDL Might Happen
Scientists have suggested several reasons why testosterone therapy could affect LDL:
- Liver metabolism: Testosterone influences how the liver processes fats and cholesterol.
- Body composition changes: TRT often increases lean muscle and reduces fat mass. These shifts can change cholesterol levels, sometimes lowering triglycerides but altering LDL or HDL.
- Hormonal balance: Testosterone interacts with other hormones such as estrogen, which also plays a role in lipid metabolism.
These mechanisms are complex, which explains why research findings vary.
Practical Takeaways
- Most men will not see a dramatic rise in LDL from testosterone therapy. Increases, if they occur, are usually modest.
- The form and dose of testosterone matter. High-dose injections may have more effect on LDL than transdermal forms.
- Individual factors play a role. Men with obesity, diabetes, or preexisting heart disease may respond differently than otherwise healthy men.
- Regular monitoring is essential. Doctors usually recommend a lipid panel before starting TRT and repeat testing every 3–6 months during the first year, then annually.
Testosterone therapy does not appear to universally raise LDL cholesterol, but small increases are possible, especially with higher doses or injectable forms. For most men, these changes are not large enough to dramatically alter heart disease risk, but for men who already have high LDL or cardiovascular disease, even small increases matter.
The safest approach is regular monitoring of cholesterol levels, working with a doctor to adjust therapy if LDL rises, and maintaining a heart-healthy lifestyle through diet, exercise, and weight management.
Does Testosterone Therapy Lower HDL ("Good Cholesterol")?
One of the most common concerns about testosterone therapy (TRT) is how it affects HDL cholesterol, often called the “good” cholesterol. HDL cholesterol plays an important role in protecting heart health. Unlike LDL (“bad” cholesterol), which can build up in blood vessels, HDL helps remove extra cholesterol from the blood and carries it back to the liver for disposal. Higher levels of HDL are usually linked with lower risks of heart disease and stroke. Because of this, doctors and patients pay close attention to how TRT influences HDL.
What the Research Shows
Many studies have looked at the effect of testosterone therapy on HDL cholesterol. Across these studies, one pattern shows up again and again: TRT often lowers HDL cholesterol levels. The drop is usually modest, but in some men, it can be more noticeable.
For example:
- Clinical trials in men receiving testosterone injections often show a 5% to 10% decrease in HDL cholesterol after several months of treatment.
- Men using testosterone gels or patches sometimes see smaller decreases, but the effect is still present.
- Long-term studies suggest that the lower HDL levels may remain steady while on therapy, though they may return to baseline if therapy is stopped.
It is important to note that these effects can differ depending on dose, delivery method, and the patient’s health status. Higher doses of testosterone, especially those used outside of medical supervision, are more likely to cause larger drops in HDL.
Why Does Testosterone Lower HDL?
The exact reasons are still being studied, but researchers believe testosterone influences HDL through several biological pathways:
- Liver metabolism: Testosterone can change how the liver processes fats, including lipoproteins like HDL.
- Enzyme activity: Testosterone may increase the activity of enzymes such as hepatic lipase, which break down HDL particles.
- Changes in fat distribution: TRT often reduces body fat and increases muscle mass. While these changes improve overall metabolism, they may also shift the balance of cholesterol particles in the blood.
These mechanisms help explain why even medically supervised testosterone therapy often results in lower HDL levels.
Why Lower HDL Matters
Lower HDL is not always dangerous on its own, but it can matter depending on a person’s overall risk profile:
- In men with otherwise normal cholesterol and low heart risk, a small drop in HDL may not significantly raise the chance of heart disease.
- In men with multiple risk factors—such as high LDL cholesterol, high blood pressure, obesity, or diabetes—a further decrease in HDL can add to cardiovascular concerns.
This is why doctors rarely look at HDL in isolation. Instead, they consider the full lipid profile (LDL, HDL, triglycerides, and total cholesterol) together with blood pressure, blood sugar, and family history of heart disease.
Differences Between Types of Therapy
Not all forms of testosterone therapy affect HDL the same way:
- Injectable testosterone: Often linked with the largest decreases in HDL, especially when given in high doses.
- Transdermal therapy (gels, patches): Usually causes smaller decreases in HDL compared to injections.
- Oral testosterone: Some older forms of oral testosterone had major negative effects on cholesterol, but modern formulations are rarely used and less studied.
These differences show that the method of treatment matters, and doctors may choose one option over another based on a patient’s cholesterol profile.
Do Lower HDL Levels Always Mean Higher Heart Risk?
This is an area of ongoing debate. For many years, doctors believed that higher HDL always meant lower heart disease risk. But more recent research suggests the relationship is more complex. Some people with naturally high HDL still develop heart disease, while others with lower HDL remain healthy.
When it comes to TRT, HDL levels may go down, but this does not always lead to higher rates of heart attacks or strokes in studies. For example, some trials have found reduced HDL without any clear rise in cardiovascular events. Other studies, however, suggest caution, especially in older men with preexisting heart disease.
The takeaway is that HDL is only one part of the story. Doctors must look at the whole patient picture before deciding if TRT is safe.
What Patients Should Know
If you are considering testosterone therapy, here are the key points about HDL cholesterol:
- TRT often lowers HDL, but the drop is usually modest.
- The effect can vary depending on the type and dose of therapy.
- A small decrease in HDL may not always mean higher heart risk, but it matters more in men with other cardiovascular risk factors.
- Regular blood tests are important. Most doctors will check cholesterol levels before starting TRT, then repeat tests at 3–6 months, and again once a year.
- Lifestyle choices—such as eating a balanced diet, exercising, and not smoking—can help support healthy cholesterol levels while on TRT.
Testosterone therapy commonly lowers HDL (“good cholesterol”), though the size of the decrease varies. This change happens because testosterone affects fat metabolism and certain enzymes in the liver. While a drop in HDL may raise concerns, the overall impact on heart health depends on the broader risk profile of the individual. For most patients, regular monitoring and a healthy lifestyle are the best ways to balance the benefits of TRT with cholesterol-related risks.
What Happens to Triglycerides on Testosterone Therapy?
When people think about cholesterol, they often focus on LDL (“bad cholesterol”) and HDL (“good cholesterol”). But there is another important fat in the blood called triglycerides. Triglycerides are the most common type of fat in the body. After you eat, your body turns extra calories into triglycerides and stores them in fat cells. Later, hormones release them to give you energy between meals.
Having high triglycerides, however, is not good for health. Very high levels are linked to heart disease, stroke, and inflammation of the pancreas (pancreatitis). Doctors often check triglycerides along with cholesterol as part of a blood test called a lipid panel.
Because testosterone therapy (TRT) can affect how the body processes fats, many people wonder: Does TRT make triglycerides go up or down? Let’s look at what the research says.
Testosterone and Lipid Metabolism
Testosterone influences the way the body uses and stores fat. It affects enzymes in the liver, muscles, and fat tissue. These enzymes control how fats like triglycerides are broken down or stored.
- In low testosterone states (such as hypogonadism), men often develop higher body fat, more insulin resistance, and unfavorable cholesterol levels—including high triglycerides.
- When testosterone levels are restored through therapy, some of these problems can improve. TRT may lower body fat, improve insulin sensitivity, and sometimes lead to better triglyceride control.
Evidence from Clinical Studies
Research findings on TRT and triglycerides are somewhat mixed, but there are several trends:
- Mild Decrease in Triglycerides
- Several clinical trials have shown that TRT leads to a small but measurable drop in triglycerides.
- The effect is usually stronger in men who had high triglycerides before starting therapy.
- On average, reductions are modest—about 5–15% in many studies.
- Greater Impact in Metabolic Syndrome
- Men with obesity, type 2 diabetes, or metabolic syndrome (a group of risk factors that includes high blood sugar, high blood pressure, and abnormal cholesterol) often see a bigger improvement in triglycerides with TRT.
- This may be because testosterone therapy helps reduce belly fat and improve insulin function, which are closely linked to triglyceride levels.
- Neutral Effect in Some Cases
- Not all studies show a benefit. In men with normal baseline triglycerides, TRT often has little or no effect.
- Some trials report no significant change in triglyceride levels, suggesting the effect depends on individual health factors.
Why Does TRT Sometimes Lower Triglycerides?
There are a few reasons why testosterone therapy might help reduce triglycerides:
- Weight and Body Fat Reduction: Testosterone therapy can increase lean muscle mass and reduce fat mass, especially in the abdomen. Less abdominal fat leads to lower triglyceride production.
- Improved Insulin Sensitivity: High insulin resistance is strongly tied to high triglycerides. TRT often improves insulin response, which can help normalize fat metabolism.
- Liver Effects: Testosterone influences how the liver produces and clears fats from the blood. Better liver function in fat handling may lead to lower triglycerides.
Does the Type of Testosterone Therapy Matter?
Different forms of TRT may affect triglycerides differently:
- Injectable testosterone: Some studies suggest injections may have a slightly stronger effect in lowering triglycerides compared to gels or patches.
- Transdermal therapy (gels/patches): Usually has a mild or neutral effect.
- Oral testosterone (rarely used): Can sometimes increase certain liver enzymes and affect fat metabolism differently, but this form is less common because of safety concerns.
Limitations of Current Research
It’s important to note that:
- Most studies are short-term (3 months to 2 years). Long-term effects of TRT on triglycerides are still being studied.
- Many trials are small and may not apply to everyone.
- Lifestyle factors—like diet, exercise, and alcohol intake—play a big role in triglyceride levels. Sometimes improvements are more related to lifestyle changes combined with TRT, rather than TRT alone.
Testosterone therapy may lower triglycerides in some men, especially those with obesity, diabetes, or high triglycerides at the start. The improvement is usually modest, and not all men experience it. TRT’s effect seems to be connected to better body composition and insulin function rather than a direct action on triglycerides alone.
While the evidence so far is encouraging, more long-term studies are needed to fully understand how TRT influences triglycerides and whether these changes reduce the risk of heart disease. For now, men on testosterone therapy should work closely with their healthcare provider, monitor their lipid panel regularly, and maintain a heart-healthy lifestyle.
Does the Type of Testosterone Therapy Matter for Cholesterol?
When talking about testosterone therapy, many people think it is all the same. But in fact, there are different ways testosterone can be given. Doctors can prescribe it as an injection, a gel or cream applied on the skin, a patch, or in some cases, oral tablets. Each method affects the body in a slightly different way, and research shows that these differences can also affect cholesterol levels. Understanding these differences can help patients and doctors make the safest choices.
Injectable Testosterone
How it works
Injectable testosterone is one of the most common forms of therapy. The hormone is injected into a muscle, usually every one to four weeks, depending on the type. The two main injectable forms are testosterone enanthate and testosterone cypionate.
Effects on cholesterol
Research suggests that injectable testosterone may lower HDL (“good cholesterol”) more than some other forms. This is important because HDL helps remove LDL (“bad cholesterol”) from the blood. Lower HDL levels can reduce protection against heart disease. At the same time, some studies show that injectable testosterone does not usually raise LDL, and in some men, it might even lower triglycerides. Still, the consistent pattern is that HDL tends to go down with injections.
Why it happens
One reason may be that injections often create “peaks and valleys” in testosterone levels. Right after an injection, levels are high, and just before the next dose, they are low. These swings may influence how the liver processes cholesterol.
Transdermal Gels and Creams
How it works
Testosterone gels or creams are rubbed on the skin daily, usually on the arms, shoulders, or abdomen. The hormone is absorbed through the skin and slowly enters the bloodstream.
Effects on cholesterol
Studies suggest that gels and creams may have a milder effect on cholesterol compared to injections. HDL might drop slightly, but usually not as much as with shots. LDL and triglycerides usually stay about the same. Some studies even show small improvements in triglyceride levels with gels.
Why it happens
Because gels give a steady supply of testosterone each day, blood levels are more stable. This steady pattern seems to have less impact on how the liver makes or clears cholesterol.
Testosterone Patches
How it works
Patches are placed on the skin, often on the back, stomach, or thighs. They release testosterone slowly over 24 hours. Like gels, they provide stable levels.
Effects on cholesterol
Patches appear to have effects similar to gels. HDL may drop a little, but usually the changes are small. LDL and triglycerides are generally not affected. Some studies show no meaningful changes at all.
Why it happens
Again, the key factor seems to be the steady hormone levels. The body is not exposed to the big spikes and drops that come with injections, and this may help protect cholesterol balance.
Oral Testosterone
How it works
Oral testosterone is less common in the United States because it can affect the liver. However, newer forms, such as testosterone undecanoate capsules, are used in some countries and are becoming more available.
Effects on cholesterol
Older oral testosterone pills were known to cause strong changes in cholesterol. They often lowered HDL and sometimes raised LDL. The liver processed these older forms directly, which had toxic effects. Newer oral forms like testosterone undecanoate are thought to be safer, but studies are still limited. Some research shows little to no effect on cholesterol, while others show HDL reduction similar to injections.
Why it happens
Even with new oral forms, the liver still plays a central role in processing the hormone. Because cholesterol is also managed by the liver, there may be crossover effects. More research is needed to know how safe newer oral testosterone is for long-term cholesterol health.
Pellets (Implants)
How it works
Testosterone pellets are small solid pieces of hormone inserted under the skin, often in the hip or buttock area. They slowly release testosterone for three to six months.
Effects on cholesterol
Research on pellets is more limited, but available studies suggest their effects on cholesterol are similar to gels and patches. HDL might fall a little, but LDL and triglycerides usually remain unchanged.
Why it happens
Pellets give a long-term, steady release of testosterone, so blood levels remain fairly stable. This may explain why cholesterol effects are mild.
Comparing the Different Forms
When looking at all the options, a clear pattern appears:
- Injections tend to lower HDL more than other forms.
- Gels, creams, patches, and pellets usually cause smaller changes, if any, in cholesterol.
- Older oral forms had strong negative effects on cholesterol, but newer oral forms may be safer, though research is still ongoing.
This does not mean injections are “bad” or that gels are “better.” The choice of therapy depends on many factors, including convenience, cost, safety, and individual health conditions. However, for patients with already low HDL or high risk of heart disease, a doctor may prefer gels, patches, or pellets instead of injections.
The type of testosterone therapy does matter when it comes to cholesterol. Injections are linked with bigger drops in HDL cholesterol, while gels, patches, and pellets seem to have gentler effects. Oral forms remain an area where more research is needed. For patients and doctors, knowing these differences is important for choosing the right therapy and planning regular cholesterol monitoring.
Does Testosterone Therapy Increase the Risk of Heart Disease?
Heart disease is one of the biggest concerns people have when they think about starting testosterone therapy (often called TRT). Because cholesterol is closely linked to heart health, many patients and doctors want to know if taking testosterone increases the chance of having a heart attack, stroke, or other heart problems. The answer is not simple. Research has shown mixed results, and many factors—such as age, type of therapy, and preexisting health conditions—play a role. Let’s look carefully at what we know from the evidence.
The Difference Between Cholesterol Changes and Real Heart Risks
First, it is important to separate cholesterol changes from actual heart disease outcomes. Testosterone therapy may affect cholesterol numbers. For example, studies often show that TRT lowers HDL (“good cholesterol”) and sometimes increases LDL (“bad cholesterol”). But a change in cholesterol does not always mean a person will develop heart disease. Many other factors—like blood pressure, blood sugar control, body weight, and lifestyle—also matter. That is why researchers study both cholesterol levels and real events, like heart attacks and strokes, to understand the full picture.
Early Studies That Raised Concerns
Some of the first studies that got public attention suggested TRT might be harmful for the heart. A 2013 study of older men, many with existing health problems, reported a higher rate of heart attacks in those taking testosterone compared to those who were not. This made headlines and created fear that TRT could raise cardiovascular risk. Another small trial in 2010 also showed more cardiovascular events in men receiving testosterone gel. These early reports led the U.S. Food and Drug Administration (FDA) in 2015 to require a warning label about possible heart risks for prescription testosterone products.
Larger and More Recent Studies
Later, larger studies did not find the same level of danger. For example, observational studies that included thousands of men found no clear increase in heart attack or stroke rates among men on TRT. Some even suggested the opposite—that men with low testosterone who received treatment had a lower risk of heart disease compared to those who stayed untreated.
In 2023, a major clinical trial called the TRAVERSE study looked specifically at whether TRT increased heart problems in men with low testosterone and high cardiovascular risk. The study followed more than 5,000 men for several years. Results showed no significant increase in heart attacks, strokes, or deaths in the testosterone group compared to the placebo group. This trial is important because it was large, carefully designed, and focused on the very group most doctors worry about—older men with heart risk factors.
Why the Results May Differ
So why do some studies show possible harm while others show safety—or even benefit? There are several possible reasons:
- Study design differences – Early studies were small, short-term, and sometimes included men who were not well monitored. Larger, longer studies tend to give more reliable results.
- Patient population – Some studies looked at very sick, elderly men with multiple health problems, while others included healthier men. Results can differ depending on who is studied.
- Dosage and delivery method – Testosterone injections, gels, and patches may affect the body differently. High doses or improper use (for example, non-medical use by athletes) may raise risks that are not seen with standard medical treatment.
- Other health changes – TRT may help reduce fat mass, increase muscle, and improve insulin sensitivity, all of which can be good for heart health. These benefits may offset small changes in cholesterol levels.
What Do Professional Guidelines Say?
Medical organizations take these mixed results into account. The Endocrine Society and the American Urological Association recommend that doctors use testosterone therapy only in men with clear clinical symptoms and low measured testosterone. They also suggest monitoring cholesterol, blood pressure, and heart health regularly during treatment. The FDA still requires caution and careful prescribing but has acknowledged recent evidence showing no clear rise in cardiovascular risk for most patients.
Who May Be at Higher Risk?
Even though large trials are reassuring, not everyone faces the same level of risk. Men with:
- Severe untreated heart failure
- Recent heart attack or stroke
- Uncontrolled high blood pressure
…may still be more vulnerable. Doctors often avoid starting TRT in these cases until the underlying condition is managed. For other men, especially those with well-controlled risk factors, testosterone therapy may be reasonably safe under medical supervision.
The current evidence suggests that testosterone therapy does not significantly increase the risk of heart disease in most men when prescribed appropriately and monitored carefully. While TRT can change cholesterol levels—sometimes lowering HDL or affecting LDL—the actual impact on heart attacks and strokes is less clear and may be neutral. Newer, larger trials show no major rise in cardiovascular events, which should reassure patients and doctors. Still, heart health should always be monitored closely, and treatment decisions should be individualized.
Do Age and Preexisting Conditions Change the Effect on Cholesterol?
Testosterone therapy (TRT) does not affect everyone in the same way. Age, health status, and underlying medical conditions can change how testosterone influences cholesterol levels. Some people may see improvements in their cholesterol profile, while others may experience negative changes. Understanding these differences helps patients and doctors make safer and more informed decisions.
Age Differences: Younger Men vs. Older Men
Younger Men with Low Testosterone
In men with true hypogonadism (a medical condition where the body does not make enough testosterone), TRT can help restore hormones to normal levels. In these younger men, therapy often improves overall metabolic health. Some studies show mild decreases in LDL cholesterol (the “bad” cholesterol) and neutral effects on triglycerides. HDL cholesterol (the “good” cholesterol) may sometimes drop, but often remains within the normal range.
Because younger men are usually healthier, their blood vessels are less likely to have plaque buildup or stiffening. As a result, small changes in cholesterol from TRT may not carry the same risk as they would in older adults.
Older Men with Age-Related Decline
For men over 50 or 60, testosterone naturally decreases with age. These men may seek TRT for symptoms like fatigue, low muscle mass, or sexual changes. However, in older adults, cholesterol and heart risk factors are already more complex.
Clinical trials in older men have found:
- HDL cholesterol often decreases slightly with TRT.
- LDL cholesterol may stay the same or increase modestly.
- Triglycerides may go down if body fat and insulin sensitivity improve.
Older men are more likely to already have heart disease, diabetes, or high blood pressure. Because of this, even small shifts in cholesterol caused by TRT can carry more weight. Doctors usually recommend closer monitoring for older adults compared to younger patients.
Obesity and Its Role
Obesity often changes how the body responds to testosterone. Fat tissue, especially around the belly, lowers natural testosterone levels. It also increases LDL and triglycerides while reducing HDL.
When obese men start TRT:
- They may see improved triglycerides, especially if TRT helps reduce fat mass.
- HDL may decrease slightly, although exercise and diet can offset this effect.
- LDL changes are inconsistent; some men see small reductions, others see no change.
The combination of obesity, low testosterone, and high cholesterol creates a cycle that increases heart risk. TRT can help break parts of this cycle, but it is not a cure on its own. Lifestyle changes remain essential.
Diabetes and Metabolic Syndrome
Diabetes and metabolic syndrome (a condition involving high blood pressure, high blood sugar, and abnormal cholesterol) often go hand in hand with low testosterone. Men with these conditions tend to have higher triglycerides and lower HDL.
Studies show that when men with diabetes start TRT:
- Triglycerides may drop, especially if blood sugar improves.
- HDL tends to decrease slightly, as in other groups.
- LDL response varies, but some evidence suggests that better insulin control reduces harmful cholesterol particles.
Because men with diabetes already face high risks of heart disease, doctors are extra cautious. TRT may improve some risk factors while worsening others. Regular cholesterol and blood sugar checks are key.
Preexisting Heart Disease
For men who already have heart disease, the relationship between TRT and cholesterol becomes more sensitive. Cholesterol changes caused by therapy might seem small, but even small shifts can matter for someone with blocked arteries or a history of heart attack.
Research shows mixed outcomes:
- Some men on TRT maintain stable cholesterol levels.
- Others may see a drop in HDL, which could reduce heart protection.
- Improvements in body composition and insulin resistance may help balance these risks.
Because of this mixed evidence, most guidelines advise caution. Men with known heart disease should only start TRT after a careful risk–benefit discussion with their healthcare provider.
Baseline Cholesterol Levels
Not everyone starts testosterone therapy with the same cholesterol profile. A man who begins TRT with already high LDL or very low HDL may respond differently than someone with normal cholesterol.
- High baseline LDL: TRT may not significantly raise LDL further, but because risk is already high, doctors watch closely.
- Low baseline HDL: TRT can make this worse, so lifestyle measures (exercise, weight loss, healthy fats) are even more important.
- High triglycerides: These often improve with TRT, especially if combined with weight reduction.
This means the “before treatment” cholesterol picture is an important predictor of what may happen on TRT.
What Role Does Lifestyle Play Alongside Testosterone Therapy?
When men start testosterone therapy, they often want to feel stronger, have more energy, or improve their quality of life. But testosterone therapy does not work in isolation. The way a person eats, moves, and takes care of their overall health can strongly affect how testosterone therapy changes cholesterol levels and heart health. Lifestyle choices such as diet, exercise, body weight, and alcohol or tobacco use can all make the effects of testosterone therapy either better or worse.
Below, we will look at the main lifestyle factors that matter most for cholesterol while on testosterone therapy.
Diet and Nutrition
The type of food a person eats has one of the biggest effects on cholesterol. Diets high in saturated fats (like fried foods, fatty meats, butter, and processed snacks) tend to raise LDL cholesterol, the so-called “bad cholesterol.” This matters because testosterone therapy sometimes lowers HDL cholesterol, the “good” kind. If HDL drops, it becomes even more important not to let LDL rise too high.
On the other hand, diets rich in vegetables, fruits, whole grains, lean proteins, and healthy fats (like those from nuts, olive oil, or fatty fish) can lower LDL and raise HDL. This kind of eating pattern is often called a “heart-healthy diet” or modeled after the Mediterranean diet.
For someone on testosterone therapy, following a healthy diet can help keep cholesterol balanced. In fact, studies show that men who combine testosterone therapy with improved nutrition often see better changes in their lipid profiles compared to men who rely on testosterone therapy alone.
Exercise and Physical Activity
Exercise is another powerful lifestyle factor that works with testosterone therapy. Regular aerobic activity, such as brisk walking, jogging, swimming, or cycling, is known to lower triglycerides and improve HDL cholesterol. Strength training, which many men start when they begin testosterone therapy, also helps increase lean body mass and improve metabolism.
When testosterone therapy increases muscle mass, exercise can help turn that into better long-term health outcomes. Exercise also reduces belly fat, which is closely linked to high LDL cholesterol and high triglycerides.
For men on testosterone therapy, combining treatment with at least 150 minutes of moderate-intensity exercise per week is strongly recommended by most doctors. This combination often results in lower cholesterol levels, better blood sugar control, and improved heart health.
Body Weight and Fat Distribution
Weight plays an important role in cholesterol changes. Being overweight or obese, especially carrying fat around the waist, is strongly linked to higher LDL and triglycerides, and lower HDL. Testosterone therapy sometimes helps reduce fat mass while increasing lean muscle, but the results are much stronger when paired with lifestyle changes.
For example, losing 5–10% of body weight through diet and exercise can significantly improve cholesterol levels. If a man is on testosterone therapy but does not change his eating habits or activity levels, weight may not change much, and cholesterol improvements may be limited. On the other hand, men who combine therapy with weight loss strategies usually see the greatest benefits.
Smoking and Alcohol Use
Cigarette smoking lowers HDL cholesterol and damages blood vessels. If testosterone therapy already lowers HDL a little, smoking can make the effect worse. Quitting smoking can raise HDL levels within weeks, which helps balance cholesterol changes from testosterone therapy.
Alcohol has a mixed effect. Moderate alcohol use (such as a glass of wine a few times per week) can sometimes raise HDL cholesterol, but heavy drinking increases triglycerides and raises heart disease risk. For men on testosterone therapy, keeping alcohol intake low or moderate is safest for cholesterol and heart health.
Sleep and Stress Management
Sleep and stress are less obvious lifestyle factors, but they also affect cholesterol and overall health. Poor sleep can raise LDL cholesterol and lower HDL. Stress can trigger unhealthy eating, weight gain, and higher blood pressure. Testosterone therapy may improve sleep and mood in some men, but combining it with good sleep habits and stress reduction techniques—such as meditation, deep breathing, or counseling—leads to better results for cholesterol and heart health.
How Lifestyle and Testosterone Work Together
Testosterone therapy can change cholesterol levels in small ways, but lifestyle is what often makes the bigger difference. A man who eats a poor diet, avoids exercise, and smokes may see his cholesterol worsen on testosterone therapy. In contrast, a man who uses testosterone therapy while following a healthy lifestyle often sees improved energy, leaner body composition, and a healthier cholesterol profile.
Doctors often recommend that men beginning testosterone therapy also receive counseling on diet, exercise, and other lifestyle factors. This is because long-term heart health depends on both the medical treatment and the personal choices a man makes daily.
Lifestyle plays a major role in how testosterone therapy affects cholesterol. Diet, exercise, body weight, smoking, alcohol use, sleep, and stress all interact with testosterone therapy. By making healthy choices, men can support the positive effects of testosterone therapy and reduce risks linked to cholesterol and heart disease.
How Often Should Cholesterol Be Monitored During Testosterone Therapy?
Monitoring cholesterol during testosterone therapy is an important part of staying safe and healthy. Testosterone replacement therapy (TRT) can change levels of LDL (“bad” cholesterol), HDL (“good” cholesterol), and triglycerides. While the changes are usually not dramatic, they can affect heart health over time. For this reason, doctors recommend regular blood tests to track cholesterol while someone is taking testosterone.
In this section, we will go over why monitoring is needed, what the medical guidelines suggest, how often testing should happen, and which patients may need closer follow-up.
Why Monitoring Cholesterol Matters on TRT
Cholesterol plays a central role in cardiovascular health.
- LDL cholesterol can build up in the arteries and increase the risk of heart attack or stroke.
- HDL cholesterol helps clear LDL from the blood and is protective.
- Triglycerides are fats in the blood that can also raise cardiovascular risk when elevated.
Studies show that testosterone therapy may lower HDL cholesterol in some men. LDL and triglycerides can also change, depending on the dose and the type of testosterone used. These shifts may not be dangerous by themselves, but when combined with other risks—such as high blood pressure, diabetes, or smoking—they can contribute to long-term heart disease.
Because TRT is usually a long-term treatment, it is not enough to check cholesterol once at the beginning. Continuous monitoring allows doctors to catch changes early and adjust therapy or recommend lifestyle changes if needed.
What Guidelines Suggest
Several professional groups provide advice on cholesterol monitoring for men on TRT.
- The Endocrine Society recommends that doctors measure cholesterol before starting therapy and then at follow-up visits.
- The American Urological Association (AUA) also suggests baseline lipid testing and routine monitoring afterward.
- Many cardiologists advise checking cholesterol more often in men who already have heart disease or metabolic conditions.
While there is no single worldwide schedule that every doctor follows, most experts agree on a few important steps:
- Check cholesterol before starting TRT. This gives a clear baseline.
- Repeat the test within the first 3 to 6 months. Early testing shows if TRT is causing quick changes.
- Continue testing once a year. Annual monitoring is the most common approach for men without major risk factors.
How Often Testing Should Happen
The exact frequency depends on the patient’s health. Here are the general approaches:
Low-Risk Patients
Men who are young, healthy, and do not have major heart risk factors may only need cholesterol checked:
- At baseline (before TRT starts)
- At 3–6 months after starting
- Then once every 12 months
Moderate-Risk Patients
Men with a few risk factors—such as being overweight, having slightly high blood pressure, or a family history of heart disease—may need testing:
- At baseline
- At 3–6 months
- At 6–12 months again
- Then once a year, unless changes appear that require closer follow-up
High-Risk Patients
Men with known heart disease, diabetes, or very abnormal cholesterol levels before TRT should have more frequent checks:
- At baseline
- At 3 months
- Every 6 months for the first two years
- Annually after that, if stable
If any major changes in cholesterol occur, the doctor may repeat tests even sooner.
Other Important Blood Tests Alongside Cholesterol
When doctors monitor cholesterol during TRT, they usually check other labs at the same time. These include:
- Liver function tests: since testosterone is processed in the liver.
- Hemoglobin and hematocrit: to watch for thickening of the blood.
- Blood sugar or A1C: especially in men with diabetes risk.
This combined approach gives a fuller picture of health and helps guide safe long-term treatment.
What Patients Can Do Between Tests
Cholesterol changes do not happen overnight. Still, there are steps patients can take between testing visits to support healthy cholesterol:
- Eat a diet rich in fruits, vegetables, lean protein, and whole grains.
- Limit foods high in saturated fat and processed sugars.
- Exercise regularly—both cardio and strength training.
- Avoid smoking and limit alcohol.
By combining TRT with healthy lifestyle habits, patients reduce the risk that cholesterol changes will become harmful.
The Role of Shared Decision-Making
It is important that patients and doctors make monitoring decisions together. Some men may prefer more frequent testing for peace of mind, even if their risk is low. Others may be comfortable with yearly checks. Open conversations ensure the monitoring plan matches the patient’s health needs and personal preferences.
What Are the Key Takeaways for Patients and Clinicians?
Testosterone therapy (TRT) is often prescribed to men who have low testosterone levels, either due to medical conditions or age-related decline. While TRT can improve energy, mood, muscle mass, and sexual function, it also raises important questions about heart health, especially cholesterol levels. Cholesterol plays a direct role in the risk of developing heart disease, so both patients and doctors want to know how TRT changes the balance of “good” and “bad” cholesterol, and what this means for long-term health.
This section brings together the main lessons from research so far, highlighting what is clear, what is uncertain, and what both patients and clinicians should keep in mind when considering or monitoring testosterone therapy.
TRT Can Change Cholesterol Levels in Measurable Ways
Research shows that testosterone therapy can influence cholesterol, but the effects are not the same for every person. Some of the most consistent findings include:
- LDL cholesterol (the “bad” kind): Some studies show that TRT may cause small increases in LDL, though the changes are often modest. Higher LDL can raise the risk of plaque buildup in arteries.
- HDL cholesterol (the “good” kind): Many studies report that TRT lowers HDL cholesterol slightly. Since HDL helps clear cholesterol from the blood, a drop in HDL could reduce heart protection.
- Triglycerides: In several trials, TRT lowered triglyceride levels, which may reduce metabolic risk for some men.
The size and direction of these changes depend on the dose, the type of testosterone used (injection, gel, patch), and the health status of the individual.
Cholesterol Changes Do Not Always Equal Heart Risk
One important point is that changes in cholesterol numbers do not automatically mean someone will develop heart disease. For example, even if HDL falls slightly, overall heart risk may not rise if LDL remains stable and other risk factors are well controlled. Likewise, improvements in weight, muscle mass, and insulin sensitivity from TRT can sometimes balance out small shifts in cholesterol.
This means that cholesterol levels are one piece of the larger heart health picture. Blood pressure, blood sugar, smoking status, body weight, and family history all play big roles.
The Impact of TRT Varies by Patient
Not every man responds to TRT in the same way. Several factors influence outcomes:
- Age: Younger men with clear hypogonadism may see different lipid changes than older men using TRT for age-related testosterone decline.
- Preexisting health conditions: Men with obesity, diabetes, or metabolic syndrome may see more improvement in triglycerides but also higher risk for HDL reduction.
- Baseline cholesterol: If a man already has high cholesterol before starting TRT, his response may differ from someone with normal cholesterol.
This means clinicians need to personalize care, rather than assuming TRT affects every patient equally.
Monitoring Is Essential
Because TRT can alter cholesterol, doctors usually recommend regular blood tests. A typical monitoring plan may include:
- Baseline testing before starting therapy (lipid panel, testosterone, blood sugar, and liver function).
- Follow-up testing after 3 to 6 months, then once or twice a year.
- More frequent monitoring for men with high cardiovascular risk, such as those with a history of heart disease, high blood pressure, or diabetes.
Monitoring helps catch changes early, so adjustments in therapy or lifestyle can be made as needed.
Lifestyle Choices Still Matter Most
Even though testosterone therapy can shift cholesterol levels, lifestyle habits often have a stronger influence. Eating a balanced diet low in saturated fat, exercising regularly, avoiding smoking, and maintaining a healthy weight all reduce cholesterol and heart risk. TRT is not a substitute for these steps. In fact, research shows men on TRT who combine treatment with healthy lifestyle changes often see better cholesterol outcomes than men who rely on TRT alone.
Shared Decision-Making Is Key
Because the research is mixed and the long-term effects are still being studied, open communication between patients and doctors is critical. Key points of discussion should include:
- Potential benefits (such as improved energy, mood, muscle strength, and sexual function).
- Possible risks (including changes in cholesterol, blood thickening, or other cardiovascular issues).
- Patient priorities (such as quality of life versus strict cholesterol goals).
Together, the patient and clinician can weigh risks and benefits, and decide whether TRT is appropriate, and how closely to monitor cholesterol during treatment.
The evidence suggests that testosterone therapy does affect cholesterol, especially HDL, but the overall impact on heart disease is still being studied. For most men, the changes are not extreme, but they are important enough to track. When combined with regular monitoring and healthy lifestyle habits, TRT can be used more safely. The key takeaway is balance: benefits in symptoms and quality of life must always be considered alongside possible cholesterol changes and heart risks.
Conclusion
Testosterone therapy is a treatment that is becoming more common, especially for men who have low testosterone either from aging or from medical conditions. Because cholesterol is a major factor in heart health, one of the most important questions patients and doctors ask is whether testosterone therapy can change cholesterol levels in a way that raises or lowers the risk of heart disease. The evidence we reviewed shows that the answer is not simple. Testosterone therapy does affect cholesterol, but the effect depends on many factors such as the type of therapy, the dose, the patient’s age, their baseline health, and whether lifestyle changes are made at the same time.
One of the clearest findings is that testosterone therapy can lower HDL cholesterol, often called the “good cholesterol.” HDL plays an important role in protecting the arteries by helping to clear out excess cholesterol. A drop in HDL is often seen in men taking testosterone, especially at higher doses. However, doctors are still debating how serious this effect is. Some studies suggest that the change is small and may not greatly increase the risk of heart problems, while others show that even a modest decrease in HDL could matter for men who already have heart disease or other risk factors.
LDL cholesterol, the “bad cholesterol,” has shown mixed results. Some men on testosterone therapy see little to no change in LDL, while others may experience a small increase or decrease depending on the form of therapy used. For example, oral testosterone has been linked to more negative effects on cholesterol compared to injections or skin gels. Injectable testosterone and transdermal patches often have a milder or more neutral effect. This shows why the delivery method matters when doctors and patients are making choices about treatment.
Triglycerides, another type of fat in the blood, may improve with testosterone therapy. Some studies show lower triglyceride levels after treatment, especially in men who also lose weight or improve insulin sensitivity while on therapy. Because high triglycerides are linked to heart disease, this may be a positive effect of testosterone. Still, more research is needed to fully understand this link.
Another major question is whether changes in cholesterol from testosterone therapy lead to actual differences in heart attack, stroke, or death. The data here are complex. Some large studies suggest that testosterone therapy does not increase major heart risks in most men when it is used carefully and with monitoring. Other studies show possible risks in older men with serious heart disease. What is clear is that cholesterol changes are only one piece of the puzzle. Blood pressure, blood sugar, body weight, and other health conditions also play important roles in heart health.
Age and existing health conditions strongly influence how testosterone affects cholesterol. A younger man with low testosterone due to a medical condition may respond differently compared to an older man starting therapy for age-related decline. Men who already have diabetes, obesity, or metabolic syndrome may have greater changes in their cholesterol and may need closer monitoring. This is why testosterone therapy should always be personalized. It is not a one-size-fits-all treatment, and what is safe for one man may not be safe for another.
Lifestyle choices also play a big role. Regular exercise, a healthy diet, and weight control can help offset possible negative effects of testosterone therapy on cholesterol. In some cases, combining therapy with lifestyle improvements may even enhance benefits, leading to lower triglycerides and better overall heart health. On the other hand, using testosterone without paying attention to diet and exercise could increase risks.
For all of these reasons, monitoring cholesterol is essential during testosterone therapy. Most medical guidelines recommend testing cholesterol before starting therapy and repeating the tests at regular intervals afterward. This allows doctors to spot any changes early and take action if needed. In some cases, this may mean adjusting the dose, switching the form of therapy, or adding medications to control cholesterol.
In summary, testosterone therapy can influence cholesterol, but the effects are complex. The most consistent finding is a decrease in HDL, while LDL and triglyceride levels can change in different ways depending on the person and the treatment. The real impact on heart disease is still being studied, and results remain mixed. What is most important for patients to understand is that testosterone therapy is not risk-free, but it can be used safely if there is careful monitoring and if lifestyle measures are in place.
Patients should always work closely with their healthcare providers when starting or continuing testosterone therapy. Decisions should be made by weighing the benefits, such as improved energy, mood, and muscle strength, against the potential risks, including changes in cholesterol and heart health. With a personalized plan, regular checkups, and attention to overall health, testosterone therapy can be managed in a way that reduces risks and supports long-term well-being.
Questions and Answers
Yes. Testosterone replacement therapy (TRT) can influence cholesterol by lowering HDL (“good” cholesterol) and sometimes lowering LDL (“bad” cholesterol) or triglycerides. The net effect varies between individuals.
Testosterone tends to stimulate liver metabolism of lipids, which can reduce circulating HDL cholesterol. Since HDL helps remove cholesterol from arteries, this reduction may be a concern for cardiovascular risk.
Some studies suggest that TRT can reduce LDL cholesterol slightly, especially in men with low baseline testosterone. However, the changes are usually modest and not consistent across all patients.
The relationship is complex. Lowering HDL could theoretically increase risk, but improvements in body fat distribution, insulin sensitivity, and triglycerides from TRT may balance or even improve overall cardiovascular health in some men.
Men with high cholesterol before starting TRT may see greater improvements in triglycerides and LDL, while those with normal cholesterol may mainly notice reductions in HDL.
Yes. Regular lipid panels (every 6–12 months) are recommended, since testosterone can shift cholesterol values, and cardiovascular risk should be managed proactively.
Absolutely. Exercise, a heart-healthy diet, weight management, and limiting alcohol can offset potential HDL reductions from TRT and support overall cardiovascular health.
Yes, if cholesterol levels become concerning. Physicians may combine TRT with statins or other lipid-lowering therapies to balance testosterone benefits with cardiovascular safety.
Some evidence suggests injectable testosterone may have stronger effects on lowering HDL compared to gels or patches, but results are mixed. The delivery method can influence lipid changes, but it’s not the only factor.
Not necessarily. If TRT significantly improves symptoms of low testosterone (like energy, mood, and muscle mass), doctors may continue therapy while managing cholesterol with lifestyle or medications. The decision depends on overall risk and benefits.