Low T and Fertility: The Hormonal Puzzle Behind Male Reproductive Health
Introduction
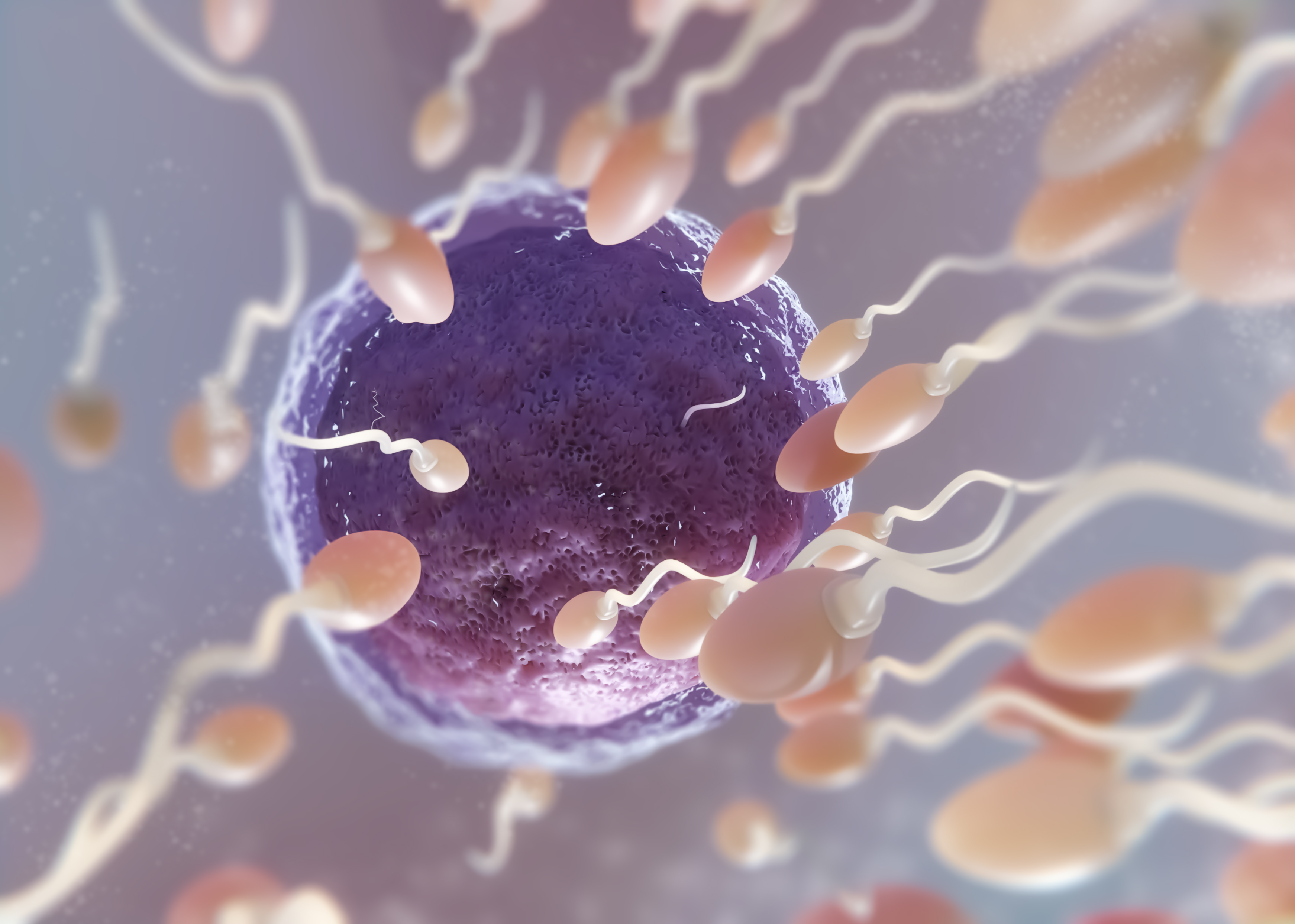
Testosterone is a hormone made mainly in the testicles. It plays a major role in many parts of a man's body. It helps with muscle growth, bone strength, sex drive, and body hair. One of its most important jobs is helping with the ability to have children. Testosterone helps make sperm, the male reproductive cells needed for fertilization. When testosterone levels fall too low, this can lead to problems with fertility and overall health.
Doctors use the term “Low T” to talk about low testosterone. Most medical experts agree that a man has Low T when his total testosterone level drops below 300 nanograms per deciliter (ng/dL). Blood tests are used to check testosterone levels, and they are usually done in the morning when hormone levels are at their highest. Low T can cause symptoms like feeling tired all the time, having a low sex drive, gaining body fat, losing muscle, feeling sad or moody, and having trouble getting or keeping an erection. Many men may not realize that these symptoms are linked to low testosterone. Even fewer may know that it can affect their ability to have children.
Fertility in men depends on healthy hormone levels and normal sperm production. Testosterone works together with other hormones, like luteinizing hormone (LH) and follicle-stimulating hormone (FSH), to help the testicles make sperm. If testosterone levels are too low, this process may not work well. This means the sperm may not develop properly, or there may not be enough sperm to fertilize an egg. Some men with Low T may not have any sperm in their semen at all, a condition known as azoospermia.
There is growing concern around male fertility today. In many parts of the world, birth rates are going down. Studies show that the average sperm count in men has dropped over the last few decades. At the same time, more men are being diagnosed with Low T. These two trends raise questions about how testosterone levels may be affecting men’s ability to start a family. People are now searching for answers about how hormones, lifestyle, and health conditions might be connected to male infertility.
More men in their 20s, 30s, and 40s are going to doctors with questions about Low T and fertility. They want to know if their symptoms could be caused by low hormone levels. They also want to know if treatments for Low T will help or hurt their chances of having a child. Many search online to learn if using testosterone therapy can restore energy and sex drive, and at the same time improve sperm quality. Unfortunately, many don’t realize that some forms of testosterone therapy can stop the body from making sperm altogether.
Doctors and researchers are still working to understand all the ways Low T affects fertility. They also look for safer treatments for men who want to feel better but still have children. Several medical treatments can help boost testosterone without harming sperm production. These include medicines that help the body make its own testosterone, instead of taking it from outside sources. Changes in diet, exercise, and sleep can also play a role in improving hormone health.
Understanding how testosterone works in the body is key to solving the puzzle of male reproductive health. Hormones are part of a complex system, and when something is off balance, it can affect more than one area of health. Low T may be one piece of the larger picture when it comes to male infertility. Knowing how to test for it, what causes it, and how to treat it safely can make a big difference for men who want to become fathers.
This article explores the most common questions asked about Low T and male fertility. It breaks down what testosterone does, how it affects sperm, and what men can do when faced with fertility issues caused by low hormone levels. Through medical facts and clear information, it will help make sense of this important topic for anyone wanting to better understand the link between Low T and fertility.
What Is Low Testosterone and How Is It Diagnosed?
Testosterone is a hormone made mainly in the testicles. It plays a key role in male development and health. Testosterone helps with muscle strength, bone growth, body hair, sex drive, and sperm production. When testosterone levels are lower than normal, the condition is called low testosterone or “Low T.”
Doctors use blood tests to check testosterone levels. Low T is usually diagnosed when the total testosterone level falls below 300 nanograms per deciliter (ng/dL). However, some men may have symptoms of low testosterone even if their levels are slightly higher than that. Because testosterone levels can change during the day, doctors usually ask for blood to be drawn early in the morning, between 7 a.m. and 10 a.m., when levels are highest.
Symptoms of Low Testosterone
Low testosterone can lead to many different symptoms. Some of the most common include:
- Low sex drive (low libido)
- Erectile dysfunction (trouble getting or keeping an erection)
- Fatigue or low energy
- Loss of muscle mass
- Increased body fat
- Mood changes, including sadness or irritability
- Trouble concentrating
- Decreased body hair or beard growth
- Lower bone density, which may lead to weaker bones
Not all men with low testosterone have all of these symptoms. Some may have only one or two. Symptoms may also be caused by other health conditions, so a proper diagnosis is important.
How Testosterone Is Measured
There are two main types of testosterone measurements: total testosterone and free testosterone.
- Total testosterone includes both the testosterone that is attached to proteins in the blood (bound testosterone) and the testosterone that is not attached (free testosterone).
- Free testosterone is the part that is not bound to proteins and is available for the body to use.
Most doctors start by measuring total testosterone. If the total level is borderline or if symptoms are strong, a free testosterone test may also be done. Free testosterone makes up only a small amount of the total (usually about 1–3%), but it is important because it is the active form the body can use.
Testosterone levels can go up and down during the day. They are usually highest in the morning and lower in the evening. Because of this, doctors recommend testing early in the morning. Also, some illnesses, medications, or even lack of sleep can affect test results. To confirm Low T, doctors usually repeat the test on two different mornings.
Other Hormone Tests
If testosterone is low, doctors often check other hormones to understand the cause. Two key hormones are:
- Luteinizing hormone (LH): This hormone is made in the pituitary gland and tells the testicles to produce testosterone.
- Follicle-stimulating hormone (FSH): Also made in the pituitary gland, FSH helps control sperm production.
If LH and FSH levels are also low, the problem may be with the brain or pituitary gland. If LH and FSH levels are high, but testosterone is low, the problem is likely in the testicles themselves.
Doctors may also test for prolactin, a hormone that can interfere with testosterone if levels are too high. In rare cases, high prolactin may point to a tumor in the pituitary gland.
Causes of Low Testosterone
Low testosterone can be caused by many different things. Some causes include:
- Aging: Testosterone levels often decrease with age.
- Obesity: Extra fat tissue can change hormone levels.
- Diabetes or metabolic syndrome
- Chronic illness, such as kidney or liver disease
- Damage to the testicles (from injury, surgery, or cancer treatment)
- Hormonal disorders or tumors
- Use of certain medications (like opioids or steroids)
Lifestyle choices such as poor diet, lack of exercise, and not getting enough sleep can also affect testosterone levels.
Why Diagnosis Matters
Diagnosing low testosterone correctly is important because the treatment depends on the cause. Giving testosterone to someone with normal levels can be harmful. Also, in men trying to have children, testosterone treatment can actually lower sperm production. That’s why doctors carefully review test results, symptoms, and medical history before making a treatment plan.
By using early morning blood tests and checking related hormones, doctors can understand whether testosterone is truly low and what might be causing it. With the right diagnosis, treatment can help improve symptoms and overall health.
How Does Testosterone Affect Male Fertility?
Testosterone is a key hormone in the male body. It plays an important role in many body functions, but it is especially important for reproduction. Testosterone helps men produce sperm, maintain a healthy sex drive, and support the function of male reproductive organs.
The process of sperm production is called spermatogenesis. This takes place in the testicles (also known as the testes). For sperm to be made properly, the body needs the right levels of testosterone in the testes. Even if the testosterone level in the blood seems normal, low testosterone inside the testicles can still cause problems with sperm production.
The Role of the Hormonal System
The male reproductive system depends on signals from the brain. The hypothalamus and the pituitary gland, located in the brain, control the levels of testosterone and other important hormones. Together, this system is known as the hypothalamic-pituitary-gonadal axis, or HPG axis.
Here’s how the system works:
- The hypothalamus releases a hormone called GnRH (gonadotropin-releasing hormone).
- GnRH tells the pituitary gland to release two hormones:
- LH (luteinizing hormone)
- FSH (follicle-stimulating hormone)
- LH travels through the blood and signals the testicles to produce testosterone.
- FSH works with testosterone to start and support the production of sperm in the testicles.
When testosterone levels are at the right balance in the testicles, sperm cells can grow and mature correctly. If testosterone is too low, sperm production slows down or stops.
Testosterone and Sperm Health
Healthy sperm is needed for a man to be fertile. Testosterone supports several things that affect sperm quality:
- Sperm count – the number of sperm in a sample of semen.
- Sperm motility – the ability of sperm to swim.
- Sperm morphology – the shape and structure of the sperm.
Low testosterone may lead to fewer sperm or sperm that do not swim well. Sometimes, it can cause azoospermia, which means no sperm is found in the semen.
Testosterone also supports the cells in the testicles that help sperm grow. These are called Sertoli cells. Without enough testosterone, Sertoli cells cannot support sperm development properly.
Libido and Sexual Function
Testosterone helps maintain libido, which means sexual desire. Low testosterone can cause a drop in sex drive, making it harder for a couple to try for pregnancy.
It also helps support erectile function. Even though testosterone is not the only factor that causes erections, low levels may contribute to erectile dysfunction, which means trouble getting or keeping an erection. This can make it difficult to have sexual intercourse, especially when trying to conceive.
Low testosterone can also cause mood changes, tiredness, and poor sleep. These changes may reduce a man’s interest or ability to take part in regular sexual activity, further affecting fertility.
Testosterone Inside vs. Outside the Testes
An important detail about testosterone and fertility is where the hormone acts. Even if a blood test shows normal or high testosterone, it may not mean there is enough testosterone inside the testicles.
Sperm production depends on very high concentrations of testosterone inside the testicles—much higher than what is needed in the bloodstream for other functions like muscle growth or mood. If the body is not making enough testosterone inside the testicles, sperm production can be impaired, even if the man does not have other symptoms.
This is why doctors often test other hormones, like LH and FSH, along with testosterone when checking for fertility problems. These tests help find out if the body is making and using testosterone correctly in the testicles.
Testosterone is vital for male fertility. It supports the entire process of sperm production, helps maintain healthy sexual function, and affects sperm quality. Without enough testosterone in the testicles, sperm may be too few, too slow, or completely absent. Understanding how testosterone works in the body helps doctors find and treat the causes of male infertility more effectively.
Can Low Testosterone Cause Infertility?
Low testosterone, also called Low T, can affect a man’s ability to have children. Testosterone is a key hormone that plays an important role in making sperm. When testosterone levels drop too low, the body may not produce enough healthy sperm for fertilization. This can make it harder or even impossible for a man to father a child.
There are different ways that low testosterone can lead to infertility. The connection depends on how low the levels are, how long they have been low, and what is causing the problem in the first place.
How Low Testosterone Disrupts Sperm Production
Testosterone is made in the testicles. It is controlled by a system called the hypothalamic-pituitary-gonadal (HPG) axis. This system starts in the brain. The hypothalamus sends a signal to the pituitary gland, which then sends hormones (LH and FSH) to the testicles. LH helps make testosterone. FSH helps make sperm. Both hormones need to be working correctly for the testicles to produce healthy sperm.
If testosterone levels fall too low, this system becomes unbalanced. The body may produce less FSH, which leads to fewer sperm. Also, low testosterone inside the testicles can stop the growth and development of sperm cells. Even if testosterone is low in the blood, the level inside the testicles must remain high for sperm to grow properly. Without enough testosterone in the testicles, sperm production may slow down or stop completely.
Primary vs. Secondary Hypogonadism
There are two main types of low testosterone that affect fertility: primary hypogonadism and secondary hypogonadism.
- Primary hypogonadism happens when the testicles are damaged or not working properly. Even if the brain sends the right signals, the testicles cannot make enough testosterone or sperm. This type of Low T is usually harder to treat. It may be caused by genetic problems (like Klinefelter syndrome), infections, injury, or past cancer treatment (like radiation or chemotherapy).
- Secondary hypogonadism happens when the problem starts in the brain. The pituitary gland or hypothalamus does not send enough signals (LH and FSH) to the testicles. As a result, the testicles do not produce enough testosterone or sperm. This type can often be reversed or improved with treatment. Causes include pituitary tumors, obesity, stress, certain medications, or anabolic steroid use.
In both cases, fertility can be affected because of low testosterone and poor sperm production. Doctors use blood tests and imaging studies to tell the difference between the two types.
Common Causes of Low Testosterone That Affect Fertility
Several health conditions and lifestyle choices can cause testosterone levels to drop. These causes often affect the brain’s ability to send signals or the testicles' ability to respond. Some examples include:
- Obesity: Fat cells convert testosterone into estrogen, which lowers T levels.
- Chronic illness: Conditions like diabetes or liver disease may interfere with hormone balance.
- Anabolic steroids: These drugs shut down the body’s natural testosterone and sperm production.
- Stress and poor sleep: Both can disrupt the HPG axis and lower testosterone.
Sometimes, men have more than one cause at the same time. For example, a man with obesity and diabetes may also be using medications that lower testosterone. When this happens, sperm production may be affected more severely.
What the Research Shows
Studies have shown that men with low testosterone are more likely to have problems with fertility. One study found that men with Low T had lower sperm counts, lower sperm motility (movement), and more sperm abnormalities. These problems can make it harder for sperm to reach and fertilize an egg.
Other studies have found that even men with testosterone levels in the lower “normal” range may have reduced fertility. This suggests that sperm production is sensitive to changes in hormone levels, even if they are not very extreme.
However, not all men with low testosterone become infertile. Some men can still produce enough healthy sperm to father children, especially if their Low T is mild or temporary. The outcome often depends on how early the problem is found and how quickly treatment begins.
Low testosterone can cause infertility by interfering with the body’s ability to make sperm. It affects the hormone signals from the brain and the function of the testicles. The causes of Low T include both medical conditions and lifestyle factors. The two main types of Low T—primary and secondary hypogonadism—affect fertility in different ways. Studies show that men with Low T often have lower sperm counts and poorer sperm quality. But with the right diagnosis and treatment, some of these problems can be managed or reversed.
Does Testosterone Replacement Therapy (TRT) Improve or Harm Fertility?
Many men think that bringing blood testosterone back to “normal” must help sperm production. The opposite is true. Most forms of TRT—shots, skin gels, long-acting pellets, or oral capsules—raise testosterone in the blood but cut off the body’s own signal to make sperm.
How the Hormonal Signal Works
The brain’s hypothalamus releases gonadotropin-releasing hormone (GnRH). GnRH tells the pituitary gland to send out two other messengers: luteinizing hormone (LH) and follicle-stimulating hormone (FSH). LH triggers the Leydig cells in the testes to make testosterone. FSH supports Sertoli cells, which guide developing sperm. High levels of testosterone inside the testes (often 50- to 100-times higher than in the blood) keep sperm formation on track.
Why External Testosterone Shuts Down Sperm
When TRT floods the bloodstream with testosterone, the hypothalamus senses “enough hormone” and slows GnRH. Pituitary LH and FSH then fall. Without LH, the testes stop making their own testosterone; without FSH support, Sertoli cells cannot finish building mature sperm. Intratesticular testosterone drops sharply even while the blood level looks perfect. The result is a steep fall in sperm count that can reach complete absence of sperm (azoospermia) in three to six months of steady therapy. Studies place the risk of azoospermia between 40 % and 90 %, with injectable formulations acting fastest because they create very high peaks in serum testosterone. pmc.ncbi.nlm.nih.govtau.amegroups.org
Differences Among Delivery Methods
- Injectable enanthate or cypionate: Peak levels are high; suppression is strong. Sperm often disappear within four months.
- Transdermal gels or patches: The rise is smoother, but steady dosing still lowers LH and FSH. Average time to azoospermia stretches to six or seven months.
- Long-acting pellets and undecanoate injections: Because the dose lasts 10–12 weeks, the pituitary stays quiet for a longer block of time, deepening suppression.
- Nasal testosterone: Short half-life may reduce, but does not remove, the risk; standard fertility trials are still few.
All routes share the same negative-feedback loop: any rise in external testosterone lowers the hormones that protect sperm production.
Recovery After Stopping TRT
Stopping therapy lets GnRH, LH, and FSH wake up, but recovery is not instant. Younger men who used TRT for less than one year often regain sperm counts within six to 12 months. Men who used it for several years, started treatment after age 40, or combined it with anabolic steroids may wait 18–24 months. About two-thirds of formerly azoospermic men regain measurable sperm within a year; the rest need longer or do not return to their old baseline. New 2024 guideline updates recommend delaying a post-TRT semen test until at least 12 months have passed, and repeating it up to three years if the first result is poor. auajournals.orgauanet.org
Medical Aids for Faster Recovery
Doctors can speed recovery by replacing the missing pituitary signals:
- Human chorionic gonadotropin (hCG): Mimics LH to restart testicular testosterone.
- Recombinant FSH: Added when sperm counts stay very low.
- Selective estrogen receptor modulators (SERMs) such as clomiphene citrate: Block estrogen feedback at the brain, lifting GnRH and both gonadotropins.
Combined hCG plus clomiphene can restore sperm in more than 70 % of cases within nine months, even after long TRT exposure. pmc.ncbi.nlm.nih.govfertstert.org
When TRT Is Contraindicated
Current endocrine and urology societies advise against starting or continuing TRT when a man wishes to father a child in the near term. Exceptions are rare and include:
- Primary testicular failure where sperm are already absent and fertility cannot be restored.
- Severe hypogonadal symptoms plus documented infertility solutions such as frozen sperm already in storage.
- Short-term use of very low-dose intranasal testosterone with close monitoring, still considered experimental.
Sperm banking before TRT and counseling about the timeline for recovery are considered best practice.
Exogenous testosterone corrects low serum testosterone but usually harms fertility because it shuts down the hormones that drive sperm growth. Most healthy men on TRT become oligospermic or azoospermic within months. Stopping therapy allows the hormonal axis to restart, yet full sperm recovery may take a year or more and is not guaranteed, especially after long treatment courses or in older patients. Fertility-friendly options such as hCG, FSH, or SERMs can help the testes make their own testosterone without blocking spermatogenesis. For men who plan to conceive, guidelines favor these alternatives over standard TRT and recommend sperm preservation before any treatment that may suppress the hypothalamic-pituitary-gonadal axis.
What Are the Fertility-Friendly Alternatives to TRT?
Testosterone Replacement Therapy (TRT) is a common treatment for men with low testosterone. It can help improve energy, mood, and sexual function. But TRT can also stop the body from making sperm. This happens because TRT sends a message to the brain that the body has enough testosterone. As a result, the brain stops making hormones that are needed for sperm production. Many men who take TRT may develop low sperm counts or even have no sperm in their semen. This makes TRT a poor choice for men who want to have children.
There are other treatments that can raise testosterone levels without harming fertility. These are called fertility-friendly treatments. They help the body make its own testosterone while also keeping sperm production active. Some of the most effective options are gonadotropins, clomiphene citrate, and aromatase inhibitors.
Gonadotropins: hCG and FSH
Gonadotropins are hormones that tell the testes to make both testosterone and sperm. Two important gonadotropins are:
- Human chorionic gonadotropin (hCG)
- Follicle-stimulating hormone (FSH)
hCG acts like luteinizing hormone (LH), which the body normally makes in the brain. It tells the Leydig cells in the testes to produce testosterone. When hCG is given through regular injections, it helps increase testosterone levels inside the testes, not just in the bloodstream. This internal testosterone is necessary for sperm production.
FSH works together with hCG to directly support spermatogenesis (the process of making sperm). It helps the Sertoli cells inside the testes grow and mature sperm.
Gonadotropin therapy is often used in men with low sperm counts or azoospermia (no sperm). It is especially useful in men with secondary hypogonadism, where the problem starts in the brain, not the testes. Treatment usually takes 3 to 6 months or longer to show results. Semen analysis is done every few months to check sperm levels.
While this treatment can be expensive and requires injections several times per week, many men are able to restore both testosterone and fertility with it.
Clomiphene Citrate
Clomiphene citrate is an oral medication that has been used for many years in both women and men with fertility problems. It belongs to a class of drugs called selective estrogen receptor modulators (SERMs). Clomiphene works by blocking estrogen receptors in the brain. This tricks the brain into thinking the body has low estrogen, which leads to increased production of LH and FSH. These hormones then stimulate the testes to make more testosterone and sperm naturally.
Clomiphene is taken as a pill, usually every other day or several times per week. It is a popular choice because it is easy to take and does not stop sperm production. In fact, it often improves sperm counts.
This medication is best for men with functional hypogonadism, which is caused by factors like obesity, stress, or certain medications. It is not as effective for men with primary testicular failure. Side effects may include mood swings, vision problems, or headaches, but most men tolerate it well.
Aromatase Inhibitors (AIs)
Aromatase inhibitors, such as anastrozole and letrozole, are pills that stop the body from converting testosterone into estrogen. Some men with low testosterone have higher estrogen levels, especially if they are overweight. Too much estrogen can lower the brain’s signal to make LH and FSH, which reduces testosterone and sperm production.
By lowering estrogen levels, aromatase inhibitors help restore the natural hormonal balance. The brain responds by making more LH and FSH, which then boost testosterone and sperm production. AIs are especially helpful in men with a low testosterone-to-estrogen ratio.
These medications are taken once or twice a week and are often used together with other fertility treatments. Like clomiphene, they are safe for fertility and do not block sperm production.
Monitoring and Success Rates
All fertility-friendly treatments need close monitoring by a doctor. Hormone levels are checked regularly. Semen analysis is done every few months to track progress. If a man is responding well, testosterone levels rise and sperm counts improve.
Success rates depend on the cause of low testosterone and the man’s overall health. Many men see good results with these therapies, especially when started early. Treatment can continue for several months or even years, depending on fertility goals.
These options give men a way to restore hormonal balance and maintain the ability to have children. They are important alternatives to TRT for men who want to keep their fertility intact.
What Are the Most Common Causes of Low Testosterone in Men of Reproductive Age?
Low testosterone, or “low T,” can happen for many reasons. In men of reproductive age, it can be caused by problems in the testicles, issues with the brain’s hormone control system, lifestyle choices, or even chemicals in the environment. Some of these causes are reversible, while others may be long-term or permanent. Understanding these causes helps doctors decide on the best treatment.
Primary Hypogonadism: When the Testicles Don’t Work Properly
One major reason for low testosterone is a condition called primary hypogonadism. This happens when the testicles themselves cannot produce enough testosterone. The brain may still be sending signals to the testicles to make testosterone, but the testicles do not respond well.
Some men are born with this condition. A genetic disorder called Klinefelter syndrome is one example. Men with this syndrome have an extra X chromosome. This causes their testicles to be smaller and work less effectively, often leading to both low testosterone and poor sperm production.
Other men may develop testicular failure later in life. This can happen from infections like mumps, injury to the testicles, or radiation and chemotherapy treatments for cancer. These conditions damage the testicular tissue that makes testosterone and sperm.
In primary hypogonadism, the levels of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the brain are often high. This is because the brain is trying hard to tell the testicles to work, but the testicles do not respond.
Secondary Hypogonadism: Problems in the Brain’s Hormone Control Center
Another major type of low testosterone is secondary hypogonadism. In this case, the problem is not with the testicles but with the brain areas that control hormone production — the hypothalamus and the pituitary gland.
These parts of the brain send signals to the testicles using LH and FSH. If the brain does not send enough of these hormones, the testicles will not make testosterone, even if they are healthy.
Pituitary tumors are one possible cause of secondary hypogonadism. These tumors can press on the part of the brain that controls hormone release. Other brain injuries, surgeries, or conditions like hemochromatosis (too much iron in the body) can also affect hormone signaling.
Some medications can lower testosterone by affecting the brain. These include opioid pain medications, steroids, and certain drugs used for depression or psychiatric conditions.
Obesity and Poor Lifestyle Habits
Obesity is a very common cause of low testosterone in men today. Fat cells in the body turn testosterone into estrogen, a hormone usually found in higher amounts in women. When men have more fat tissue, more of their testosterone gets turned into estrogen, leading to lower testosterone levels.
Obesity also increases inflammation in the body. This can interfere with the signals between the brain and the testicles. In addition, men who are overweight or obese often have poor sleep and lower physical activity, both of which can also lower testosterone.
Lack of exercise, poor diet, and chronic stress can make the problem worse. Stress causes the body to release cortisol, a hormone that blocks testosterone production.
Environmental Chemicals and Endocrine Disruptors
Certain chemicals in the environment can also lower testosterone. These chemicals are called endocrine disruptors because they interfere with the body’s hormone systems.
Common sources of endocrine disruptors include plastics (especially those with BPA), pesticides, and industrial chemicals. These substances can act like hormones or block hormone signals. Long-term exposure may reduce testosterone levels and hurt sperm production.
These chemicals are found in some food containers, personal care products, and even in household dust. Researchers continue to study how much these chemicals affect male fertility, but there is growing concern.
Medical Conditions That Lower Testosterone
Some chronic medical conditions can lower testosterone levels as well. These include:
- Type 2 diabetes
- Chronic kidney disease
- Liver disease
- Sleep apnea
- HIV/AIDS
These health problems can affect hormone levels directly or cause inflammation that interferes with testosterone production. Treating these conditions may help improve hormone balance.
Low testosterone in men of reproductive age can come from several causes. Problems with the testicles, issues in the brain’s hormone centers, lifestyle factors, chemical exposure, and chronic illnesses all play a role. Some causes are treatable and reversible, while others may require ongoing care. A full medical evaluation can help find the exact cause and guide the best treatment to protect both hormone health and fertility.
How Is Low Testosterone Evaluated in Men with Infertility?
When a man has trouble fathering a child, doctors may check for low testosterone as part of a full fertility exam. Testosterone plays a key role in sperm production, so low levels can affect the ability to have children. To understand the cause of infertility and plan treatment, doctors use several steps to evaluate hormone levels and other health factors.
Semen Analysis
A semen analysis is often the first test done when a man is being checked for infertility. This test measures the number of sperm, how they move, and how they look. It also shows if sperm are present at all. A normal semen analysis usually shows a sperm count of over 15 million sperm per milliliter, good movement (motility), and normal shape (morphology).
If the test shows a low sperm count or no sperm (azoospermia), it could be linked to low testosterone or other problems with the testicles. Doctors may repeat the semen analysis once or twice, since sperm levels can change over time.
Hormone Testing
Hormone tests are key to finding out if low testosterone is causing infertility. Blood tests are usually taken early in the morning, when testosterone is highest. Doctors often check the following hormone levels:
- Total Testosterone (T): Measures all testosterone in the blood, both bound and free. A level below 300 nanograms per deciliter (ng/dL) is usually considered low.
- Free Testosterone: This is the portion of testosterone that is not attached to proteins and is available to the body. It may be measured if total testosterone is borderline or symptoms are present.
- Luteinizing Hormone (LH): This hormone from the brain controls testosterone production in the testicles. Low LH with low T may point to a brain (pituitary) problem, while high LH suggests the testicles are not responding.
- Follicle-Stimulating Hormone (FSH): This hormone helps the body make sperm. High FSH may mean that the testicles are not producing sperm well.
- Prolactin: A high prolactin level can lower testosterone and sperm production. High levels may suggest a tumor in the pituitary gland.
- Estradiol: This form of estrogen is sometimes high in men with obesity or other hormone imbalances. High estradiol can reduce testosterone and harm fertility.
These hormone tests help doctors understand where the problem is—in the testicles, the brain, or both.
Imaging Studies
If the hormone tests show low LH and FSH, doctors may check for a problem in the brain. A pituitary MRI (magnetic resonance imaging) may be done to look for tumors or other changes in the pituitary gland, which controls hormone release. This type of tumor is usually noncancerous, but it can press on nearby areas and lower hormone levels.
For men with no sperm or very low sperm counts, a scrotal ultrasound can check for physical problems in the testicles or blockages in the sperm ducts. It can also spot signs of varicoceles—swollen veins in the scrotum—which can lower sperm quality and testosterone levels.
Genetic Testing
If a man has very low sperm count or no sperm, especially with high FSH, doctors may check for genetic causes. A karyotype test looks at the number and shape of chromosomes. Some men with infertility may have extra chromosomes, such as in Klinefelter syndrome (47,XXY). Another test called Y chromosome microdeletion testing can find missing parts of DNA that are needed for sperm production.
These tests are important because genetic problems may affect treatment choices and a couple’s options for having a child.
Full Evaluation and Diagnosis
To get a clear diagnosis, all the test results are put together. This includes semen analysis, hormone levels, imaging, and possibly genetic tests. The findings help doctors decide if the problem is in sperm production, hormone control, or a blockage.
Some men have primary hypogonadism, meaning the testicles do not work well. Others have secondary hypogonadism, meaning the brain is not sending the right signals. Still others may have both problems.
Understanding the cause is the first step toward treatment. Men with low testosterone and infertility should be fully evaluated before starting any therapy, especially testosterone replacement, which can further reduce sperm production. Careful testing helps make sure the right treatment plan is used to improve both hormone levels and fertility.
Can Low Testosterone Be Prevented or Reversed Naturally?
Low testosterone, also called Low T, can happen for many reasons. Sometimes it is caused by illness or damage to the body. But in other cases, it can be linked to lifestyle habits. There are ways to support healthy testosterone levels naturally, especially for men with mild or early changes in hormone levels. While not every case of Low T can be reversed, some improvements may be possible without medication.
Healthy Weight and Body Fat
Extra body fat, especially around the stomach, is linked to lower testosterone. Fat tissue turns testosterone into estrogen. As estrogen levels go up, testosterone levels go down. This hormonal shift can also lower sperm count and affect fertility. Obesity can also raise insulin levels and increase inflammation, both of which can reduce testosterone.
Losing weight through diet and exercise can help restore hormone balance. Even a 5% to 10% weight loss can improve testosterone levels. Eating fewer processed foods and sugary drinks and choosing more vegetables, whole grains, lean protein, and healthy fats is a good place to start. Regular meals and balanced nutrition help keep insulin and blood sugar steady, which also supports hormone health.
Exercise and Physical Activity
Physical activity is one of the best ways to support testosterone. Both strength training and aerobic exercise improve hormone levels. Lifting weights increases muscle mass and can help raise testosterone, especially when done 2 to 3 times a week. High-intensity interval training (HIIT) has also been shown to boost testosterone for short periods after workouts.
Exercise helps reduce body fat, lowers stress, and supports better sleep—all of which help the body make more testosterone. However, very intense or long workouts without rest may have the opposite effect and lower hormone levels. Rest days and proper recovery are important.
Sleep and Testosterone
Testosterone is made mostly at night during deep sleep. Poor sleep or not getting enough rest can lower testosterone levels, even in healthy men. Studies show that sleeping fewer than 6 hours per night may reduce testosterone by up to 15%. This effect can happen quickly, even in just one week of short sleep.
Most adults need between 7 and 9 hours of sleep each night. Good sleep habits include going to bed at the same time every night, avoiding screens before bedtime, and creating a quiet, dark, and cool sleeping space. Limiting caffeine and alcohol can also help improve sleep quality.
Reducing Alcohol and Substance Use
Too much alcohol can lower testosterone. It affects the liver, which plays a role in hormone balance, and it can damage the testicles where testosterone is made. Heavy drinking can also reduce sperm quality and sexual function.
Smoking and using other substances like marijuana or anabolic steroids can also reduce testosterone levels. Quitting these habits can lead to improvements in hormone health and fertility over time.
Diet and Nutrients That Support Testosterone
Some nutrients play a role in testosterone production:
- Zinc is important for the cells in the testes that make testosterone. Low zinc levels can reduce testosterone. Foods like meat, shellfish, nuts, and whole grains are good sources of zinc.
- Vitamin D helps with testosterone production. Many people have low vitamin D, especially in the winter or in areas with little sunlight. Safe sun exposure and foods like fatty fish, eggs, and fortified milk can help. In some cases, vitamin D supplements may be needed.
- Healthy fats, especially from nuts, seeds, avocados, and olive oil, are needed for making hormones like testosterone. Very low-fat diets may lead to lower hormone levels.
It is important to note that while a healthy diet can support testosterone, taking large doses of supplements without medical advice is not safe. Some over-the-counter testosterone boosters may contain harmful ingredients or interfere with natural hormone production.
Supplements and Herbal Products
Many products claim to boost testosterone, but not all are proven or safe. Some herbs like fenugreek, ashwagandha, and tongkat ali have been studied, but results are mixed. Some small studies show a possible increase in testosterone, while others show no effect. These products may also interact with medications or cause side effects.
Before using any supplement, it is important to check with a healthcare provider. A doctor can test hormone levels and help decide what steps are helpful or necessary.
Stress Management
Chronic stress raises cortisol, a hormone that can lower testosterone. Long-term stress can affect sleep, mood, and weight, all of which play a role in hormone balance. Finding healthy ways to manage stress—such as breathing exercises, yoga, hobbies, or talking to a counselor—can help improve both physical and mental well-being.
In many men, small changes to daily habits can lead to better hormone balance. Regular exercise, healthy eating, restful sleep, and avoiding harmful substances can support testosterone and improve fertility. While these steps may not cure Low T in all cases, they are important for overall health and may reduce the need for medication in some men.
What Is the Outlook for Men with Low T and Fertility Challenges?
Many men with low testosterone (Low T) worry about their ability to have children. This concern is understandable, but the outlook is often better than it may seem at first. The outcome depends on several factors, including the cause of Low T, how long it has been present, and how it is treated.
Reversibility Depends on the Cause
Some men have what doctors call functional hypogonadism. This means their Low T is not due to damage to the testes or brain. Instead, it may be caused by things like obesity, stress, poor sleep, or certain medications. In these cases, hormone levels may return to normal if the underlying issue is fixed. For example, losing weight or stopping a medication can often help bring testosterone levels back up. When testosterone improves, sperm production often improves too. This makes fertility more likely.
Other men have primary hypogonadism, which means the testes cannot produce enough testosterone, no matter what the brain tells them to do. This is often due to damage from injury, infection, or a genetic condition like Klinefelter syndrome. In these cases, the Low T is usually permanent. This can also affect sperm production in a serious way. Fertility treatments may still help, but natural recovery is unlikely.
There is also secondary hypogonadism, where the problem comes from the brain (hypothalamus or pituitary gland). This can happen due to tumors, head injuries, or other diseases. Sometimes, medications or hormone therapy can restart the body’s normal signals and help improve testosterone and fertility. A fertility specialist can help find the right approach based on test results.
Early Detection Leads to Better Outcomes
Catching Low T early can make a big difference. When it is found and treated before sperm production shuts down completely, the chances of restoring fertility are much higher. Doctors often use blood tests and semen analysis to check both hormone levels and sperm health. Imaging studies, like a scrotal ultrasound or a brain MRI, may also be used to find out what is causing the problem.
When Low T is treated the right way—without using testosterone replacement therapy (TRT) that can shut down sperm production—many men go on to father children. Treatments like hCG injections or clomiphene citrate pills can help the testes make more testosterone and sperm naturally. These are especially helpful in cases of secondary hypogonadism.
Fertility Preservation Options
For some men, sperm production may already be very low or absent. In these situations, sperm banking (freezing sperm for later use) can be a smart choice. This is often recommended before starting treatments like TRT, chemotherapy, or radiation, which may lower sperm count even more. If sperm cannot be found in the semen, doctors can sometimes retrieve it directly from the testes using a small surgery. This sperm can then be used in assisted reproduction methods like IVF (in vitro fertilization).
Men who plan to delay having children should consider sperm freezing early, especially if they have Low T or other risk factors.
Mental and Emotional Health Also Matter
Low testosterone can affect more than just the body. It may lead to low mood, anxiety, or loss of confidence. When fertility problems are added to the mix, the emotional toll can be even greater. It is important to recognize these challenges and get the right support. Talking to a counselor, support group, or mental health professional can help. Reducing stress and improving mental health may also help improve hormone levels over time.
Fertility is not just a physical process—it also involves hopes, plans, and emotions. Caring for both the body and the mind can lead to better results.
Ongoing Research and Future Hope
New treatments and research are helping doctors better understand Low T and fertility. Scientists are studying safer ways to raise testosterone without harming sperm production. There is also growing interest in how diet, exercise, and environmental factors affect hormone health.
As science moves forward, more men will have better options to protect their fertility, even if they have Low T. With early testing, proper treatment, and good support, many men can reach their goal of starting or growing a family.
Conclusion
Low testosterone is a real and growing concern for many men, especially those who are trying to start a family. It can have a serious impact on reproductive health, but with the right understanding and care, it is possible to manage this condition and improve the chances of having children.
Testosterone plays a key role in many parts of male health, but it is especially important for sperm production and fertility. When testosterone levels are too low, the body may not produce enough healthy sperm. This can make it harder or even impossible for a man to father a child. Low testosterone can also lead to other symptoms like low energy, poor mood, and reduced sex drive. These issues can add stress to relationships and lower a man’s overall quality of life.
It is important to know that low testosterone and infertility are connected, but they are not the same thing. A man can have low testosterone and still be fertile in some cases. On the other hand, some men may have normal testosterone levels but still have problems with fertility for other reasons. This is why careful testing is needed to find out the exact cause of fertility problems.
Proper diagnosis involves more than just checking testosterone levels. A full hormone panel is usually needed. This includes tests for luteinizing hormone (LH), follicle-stimulating hormone (FSH), prolactin, and estradiol. A semen analysis is also very important to check how many sperm are present, how well they move, and if they look normal. Sometimes, doctors will also do imaging tests or check for genetic problems if the basic tests do not explain the cause of infertility.
One major point of confusion is the use of testosterone replacement therapy, or TRT. Many people think that taking testosterone will help men become more fertile. In reality, the opposite is true. When testosterone is given from outside the body, it can signal the brain to stop making the hormones that help the testes produce sperm. This can lead to a sharp drop in sperm count, and in many cases, sperm production stops completely. This is why men who want to have children should not use TRT unless it is clearly recommended by a specialist and fertility is not a concern.
For men who want to boost their testosterone levels and still protect or improve fertility, other treatments are available. Medications like clomiphene citrate and human chorionic gonadotropin (hCG) can help the body make more of its own testosterone while also supporting sperm production. These treatments work by stimulating the brain to send signals to the testes. In many cases, they can lead to better hormone balance and improved sperm counts over time.
There are also lifestyle changes that can support natural testosterone production and overall fertility. Keeping a healthy weight, eating a balanced diet, sleeping well, and staying active are all helpful. Reducing stress, avoiding too much alcohol, and quitting smoking or drug use can also make a big difference. While these steps do not always raise testosterone to normal levels on their own, they support overall hormonal health and can improve treatment outcomes.
The outlook for men with low testosterone and fertility problems depends on the cause and how early the issue is treated. Some men have temporary hormone problems that improve with lifestyle changes or medication. Others may have more serious conditions that need longer treatment or even sperm retrieval methods for assisted reproduction. In all cases, early testing and a clear plan can make a big difference.
Men who are worried about their testosterone or fertility should seek help from a qualified doctor. A reproductive endocrinologist or urologist with experience in male infertility can provide proper testing and advice. Emotional support is also important. Fertility struggles can be hard on mental health, and it helps to have support from a partner, counselor, or support group.
Research into male fertility and hormone health is ongoing. New treatments and tools are being developed to help more men become fathers. The connection between low testosterone and fertility is complex, but understanding the basics and taking action early can lead to better outcomes for many men and their families.
Questions and Answers
Low testosterone is a condition where the body produces less testosterone than normal, often defined as total testosterone levels below 300 ng/dL.
Yes, low testosterone can impair sperm production and reduce fertility, though it’s not the only factor involved in male infertility.
No, TRT can actually decrease sperm production by suppressing the brain’s signal to the testes, potentially worsening fertility.
Symptoms include low libido, fatigue, decreased muscle mass, mood changes, and difficulty with erections.
Testosterone is crucial for the function of Sertoli cells in the testes, which are essential for sperm development.
Yes, many men with low testosterone can still be fertile, especially if the condition is mild or managed properly.
Clomiphene citrate, hCG injections, and aromatase inhibitors can boost testosterone while maintaining or improving sperm production.
A blood test measuring total and sometimes free testosterone levels, ideally in the morning, is used to diagnose Low T.
Exercise, weight loss, better sleep, stress reduction, and a healthy diet can naturally boost testosterone levels.
Yes, if there are signs of low libido, fatigue, or fertility issues, checking testosterone levels can be part of a broader fertility evaluation.