TRT and Fatty Liver: Comprehensive Guide to Treatment and Prevention
Introduction
Testosterone Replacement Therapy (TRT) is a treatment used to help men with low testosterone levels. Testosterone is a hormone that plays a key role in many body functions. It affects muscle mass, bone density, red blood cell production, and mood. When men have low levels of testosterone, they might experience symptoms like fatigue, depression, and a decrease in libido. TRT can help alleviate these symptoms by restoring testosterone levels to a normal range.
Fatty liver disease, on the other hand, is a condition where excess fat builds up in the liver. There are two main types of fatty liver disease: Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD). NAFLD is more common and is not related to alcohol consumption. It is often linked to obesity, type 2 diabetes, and metabolic syndrome. AFLD is caused by heavy alcohol use. Fatty liver disease can lead to more serious liver conditions if left untreated, such as liver inflammation, fibrosis, and cirrhosis.
Understanding the link between TRT and fatty liver disease is important for those considering or currently undergoing TRT. Some studies suggest that TRT can affect liver health, both positively and negatively. This makes it essential to explore how TRT impacts the liver, especially in patients who may already be at risk for fatty liver disease.
The purpose of this article is to provide a comprehensive guide on TRT and fatty liver disease. We aim to answer common questions and provide clear, evidence-based information. This article will help you understand the basics of TRT and fatty liver disease, how they are connected, and what you can do to manage and prevent liver issues while on TRT.
We will begin by explaining what TRT is and why it is used. Then, we will cover the basics of fatty liver disease, including its causes, symptoms, and how it is diagnosed. After that, we will discuss the connection between TRT and fatty liver, focusing on how TRT can impact liver function. We will also identify who is at risk for developing fatty liver disease while on TRT and provide preventive measures to reduce this risk. Additionally, we will outline treatment strategies for those who already have fatty liver disease and are undergoing TRT. Managing TRT while dealing with fatty liver will be covered in detail, emphasizing the importance of coordinated care with healthcare providers.
Furthermore, we will look into future directions and research related to TRT and liver health. This will include emerging studies and potential new therapies that could benefit patients. Finally, we will conclude with a summary of key points and encourage further discussion and consultation with healthcare providers to ensure the best outcomes for those on TRT.
This guide is designed to be easy to read and understand, using simple language to ensure that complex medical information is accessible to everyone. By the end of this article, you will have a thorough understanding of how TRT and fatty liver disease are related and what steps you can take to maintain your liver health while receiving TRT.
Understanding these concepts is crucial for making informed decisions about your health. Whether you are considering TRT or are already on it, knowing how it can affect your liver is key to preventing complications and achieving the best possible health outcomes. We hope this guide provides the information you need to navigate TRT and manage or prevent fatty liver disease effectively.
What is TRT (Testosterone Replacement Therapy)?
Testosterone Replacement Therapy (TRT) is a medical treatment designed to boost the levels of testosterone in men who have low levels of this hormone. Testosterone is a crucial hormone that plays a significant role in male health. It affects muscle mass, bone density, red blood cell production, and sexual function. When a man's body does not produce enough testosterone, it can lead to various health problems. TRT aims to restore normal levels of testosterone in the body, helping men feel better and improve their overall health.
Common Indications for TRT
Doctors prescribe TRT for several reasons. The most common reason is hypogonadism, a condition where the body does not produce enough testosterone. This can be due to problems with the testicles, the pituitary gland, or other parts of the body that regulate hormone levels. Symptoms of low testosterone include fatigue, depression, reduced muscle mass, increased body fat, and a decreased interest in sex. By raising testosterone levels, TRT can help alleviate these symptoms and improve the quality of life.
Types of TRT
There are several ways to administer TRT, and the method chosen depends on the patient's needs and preferences. Here are the main types:
Injections
Testosterone can be injected directly into the muscles. This method is often done every 1 to 2 weeks. Injections are usually given in a doctor's office, but some patients learn to do them at home. This method ensures a steady release of testosterone into the bloodstream.
Skin Patches
Skin patches are applied to the skin daily. These patches slowly release testosterone into the body through the skin. They are easy to use and can be applied to different areas of the body, such as the back, abdomen, upper arms, or thighs.
Gels
Testosterone gels are applied to the skin, usually on the shoulders, upper arms, or abdomen. The gel is absorbed through the skin, providing a steady release of testosterone. Patients need to be careful to avoid skin-to-skin contact with others until the gel has dried to prevent transferring the medication.
Oral Tablets and Capsules
Oral tablets and capsules are taken by mouth. This method is less common because the liver can break down testosterone before it is absorbed into the bloodstream, making it less effective. However, newer formulations have improved absorption rates.
Pellets
Testosterone pellets are small implants inserted under the skin, usually in the buttocks or hip area. The pellets release testosterone slowly over a period of 3 to 6 months. This method provides a consistent hormone level and is convenient for patients who prefer not to deal with daily or weekly treatments.
Safety and Monitoring
Before starting TRT, it is essential to have a thorough medical evaluation. This includes blood tests to measure testosterone levels and to check for other conditions that could cause similar symptoms. Regular monitoring is also necessary during TRT to ensure the treatment is effective and to adjust the dosage if needed. Blood tests are typically done every few months to check testosterone levels, red blood cell count, and other important markers.
Potential Side Effects
Like any medical treatment, TRT can have side effects. Some common side effects include acne, sleep apnea, an increase in red blood cell count, and prostate enlargement. There is also ongoing research about the long-term risks of TRT, such as its impact on heart health and the risk of prostate cancer. It is crucial to discuss these potential risks with a healthcare provider before starting TRT.
Benefits of TRT
Many men experience significant benefits from TRT. These benefits include increased energy levels, improved mood, better sexual function, and enhanced muscle mass and strength. TRT can also help with bone density, reducing the risk of fractures and osteoporosis. Each patient's experience with TRT is unique, and the benefits often outweigh the risks for those with clinically low testosterone levels.
TRT is a treatment designed to restore normal testosterone levels in men with low levels of this important hormone. There are various methods to administer TRT, each with its advantages and potential side effects. Proper medical evaluation and regular monitoring are essential to ensure the treatment is safe and effective.
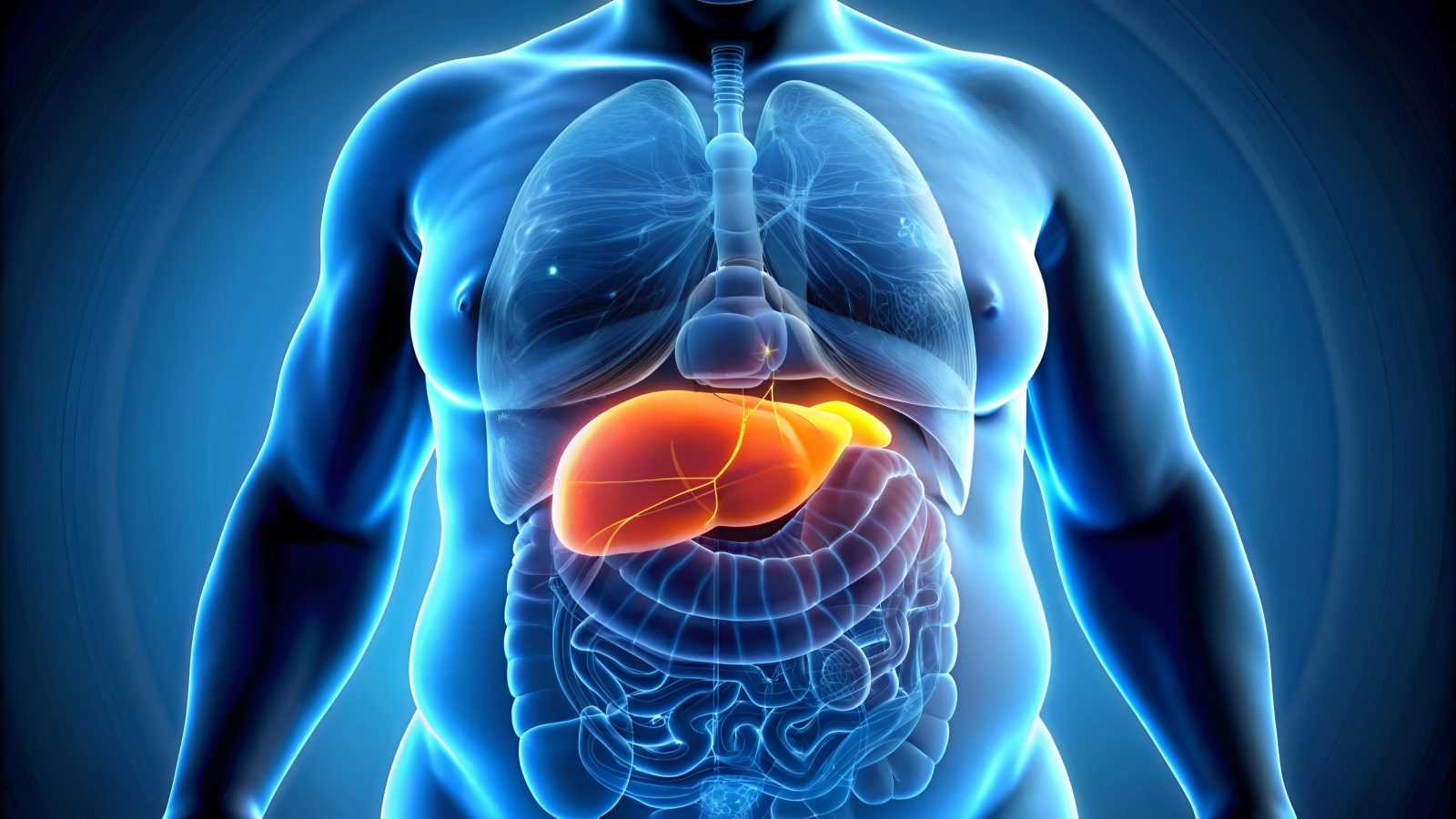
Understanding Fatty Liver Disease
Fatty liver disease, also known as hepatic steatosis, is a condition where excess fat builds up in the liver. The liver is a vital organ that processes nutrients, filters toxins, and produces bile for digestion. When it contains too much fat, it can’t function properly. Fatty liver disease is categorized into two main types: Non-Alcoholic Fatty Liver Disease (NAFLD) and Alcoholic Fatty Liver Disease (AFLD).
Non-Alcoholic Fatty Liver Disease (NAFLD):
NAFLD occurs when fat builds up in the liver of people who drink little or no alcohol. It is the most common type of fatty liver disease and is often linked to obesity, type 2 diabetes, and metabolic syndrome. NAFLD can progress to a more serious condition called Non-Alcoholic Steatohepatitis (NASH), where the liver becomes inflamed and damaged.
Alcoholic Fatty Liver Disease (AFLD):
AFLD is caused by heavy alcohol consumption. Alcohol is processed in the liver, and too much of it can cause fat to accumulate. If alcohol intake continues, AFLD can progress to more severe liver damage, such as alcoholic hepatitis and cirrhosis.
Prevalence and Risk Factors
Fatty liver disease is a widespread condition affecting millions of people worldwide. NAFLD is especially common, affecting about 25% of the global population. AFLD is also common among people who drink heavily.
Risk Factors for NAFLD:
- Obesity: Excess body weight is a significant risk factor. Fat can build up not only around the waist but also in the liver.
- Type 2 Diabetes: High blood sugar levels can lead to fat accumulation in the liver.
- Metabolic Syndrome: This includes a cluster of conditions like high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels.
- Insulin Resistance: When the body doesn’t respond well to insulin, it can lead to higher levels of fat in the liver.
- High Cholesterol and Triglycerides: These fats in the blood can also lead to fatty liver.
Risk Factors for AFLD:
- Heavy Alcohol Consumption: Drinking large amounts of alcohol over a long period is the primary risk factor.
- Gender: Women may be more susceptible to alcohol-related liver damage than men.
- Genetics: Some people may have a genetic predisposition to alcohol-induced liver disease.
Symptoms and Diagnosis
Fatty liver disease often has no symptoms, especially in the early stages. This can make it hard to detect without medical tests. When symptoms do occur, they can include:
- Fatigue: Feeling unusually tired and weak.
- Pain or Discomfort: A dull or aching pain in the upper right abdomen.
- Weight Loss: Unexplained weight loss without trying.
- Jaundice: Yellowing of the skin and eyes (more common in severe cases).
- Swelling: Swelling in the abdomen and legs (in advanced stages).
Diagnosis of Fatty Liver Disease:
To diagnose fatty liver disease, doctors use a combination of medical history, physical exams, and tests:
- Medical History: The doctor will ask about alcohol use, diet, exercise habits, and any medical conditions like diabetes or high blood pressure.
- Physical Exam: The doctor may check for signs of liver disease, such as an enlarged liver.
- Blood Tests: These can check for liver enzymes and other substances that might indicate liver damage.
- Imaging Tests: Ultrasound, CT scans, or MRI can show the amount of fat in the liver. FibroScan is a special ultrasound that measures liver stiffness, which can indicate fibrosis or scarring.
- Liver Biopsy: In some cases, a small sample of liver tissue is taken and examined under a microscope to check for inflammation and damage.
Early detection of fatty liver disease is crucial for effective management and treatment. By understanding the types, prevalence, risk factors, symptoms, and diagnosis, individuals can take proactive steps to protect their liver health.
The Link Between TRT and Fatty Liver
Testosterone is a hormone that plays a key role in many body functions, including liver metabolism. Liver metabolism is the process by which the liver processes and breaks down substances in the body. Testosterone affects how the liver handles fats and sugars, which are crucial for overall health. When a person undergoes Testosterone Replacement Therapy (TRT), they receive doses of testosterone to balance low levels of the hormone. This can influence the liver in several ways.
One way testosterone affects the liver is by altering how fats are processed. Normally, the liver helps to break down fats and remove them from the bloodstream. Testosterone can increase the liver's ability to do this, which may lead to a decrease in fat buildup. However, if the liver is already struggling due to fatty liver disease, TRT might either help improve the condition or make it worse, depending on individual circumstances.
Another important aspect is the effect of testosterone on insulin sensitivity. Insulin is a hormone that helps control blood sugar levels. Testosterone can improve insulin sensitivity, which means the body uses insulin more effectively. Better insulin sensitivity can reduce fat accumulation in the liver. However, if TRT is not carefully monitored, it might lead to imbalances that could affect the liver negatively.
Clinical Studies and Findings
Several clinical studies have explored the relationship between TRT and fatty liver disease. These studies aim to understand whether TRT is beneficial or harmful to individuals with fatty liver.
One key study found that men with low testosterone levels often have a higher risk of developing non-alcoholic fatty liver disease (NAFLD). This type of fatty liver disease is not related to alcohol consumption and is quite common. The study suggested that TRT might help reduce liver fat in these men by improving their metabolic health. For example, TRT was shown to decrease liver fat content and improve liver enzyme levels in some patients.
Another study focused on the long-term effects of TRT on liver health. It found that while TRT can improve liver function in some patients, it can also lead to complications in others. For instance, some men experienced elevated liver enzymes, which can indicate liver stress or damage. This underscores the importance of regular monitoring and careful management by healthcare providers.
Clinical findings are mixed. While TRT has the potential to improve liver health by reducing fat and improving metabolism, it also carries risks. Individual responses to TRT can vary widely, making personalized medical advice and monitoring essential.
Potential Risks and Benefits
Understanding the potential risks and benefits of TRT for individuals with fatty liver is crucial. On the one hand, TRT can offer significant health improvements. It can enhance energy levels, muscle mass, and overall quality of life for men with low testosterone levels. For the liver, the potential benefits include reduced fat accumulation, improved insulin sensitivity, and better liver enzyme profiles.
On the other hand, there are notable risks. One major concern is that TRT can sometimes increase red blood cell production, which can thicken the blood and increase the risk of blood clots. For people with fatty liver disease, this could complicate their condition. Additionally, as mentioned earlier, TRT might elevate liver enzymes, indicating liver stress.
Moreover, not all patients respond to TRT in the same way. Factors such as age, overall health, and the presence of other medical conditions can influence the outcomes of TRT. For example, older adults or those with significant liver damage might face higher risks.
Given these potential risks and benefits, it is vital for anyone considering TRT to have a thorough medical evaluation. This includes assessing liver function and discussing potential impacts with a healthcare provider. Regular follow-up appointments and liver function tests are essential to ensure that TRT is providing benefits without causing harm.
The link between TRT and fatty liver is complex. While TRT can potentially improve liver health by reducing fat and enhancing metabolism, it also carries risks that must be carefully managed. Ongoing research and individualized medical care are key to maximizing the benefits of TRT while minimizing its risks for those with fatty liver disease.
How Does TRT Affect Liver Function?
Testosterone Replacement Therapy (TRT) can have various effects on liver function. Understanding these effects is important for anyone considering or currently undergoing TRT. This section explores the impact of TRT on liver enzymes, changes in liver fat content, and the long-term implications for liver health.
Impact on Liver Enzymes
Liver enzymes are proteins that help the liver perform its functions. Common liver enzymes include alanine transaminase (ALT) and aspartate transaminase (AST). These enzymes are often measured in blood tests to check liver health. When liver cells are damaged, these enzymes leak into the bloodstream, causing elevated levels.
TRT and Liver Enzyme Levels:
- Normal Variations: Some studies show that TRT can cause mild increases in liver enzyme levels. These changes are usually within normal limits and do not indicate serious liver damage.
- Clinical Monitoring: Regular blood tests are essential for those on TRT to monitor liver enzyme levels. If the enzymes rise significantly, it may signal liver stress or damage, requiring medical attention.
Why Liver Enzyme Levels Change:
- Hormonal Influence: Testosterone can influence liver metabolism, affecting how the liver processes fats, proteins, and other substances. This can sometimes lead to mild increases in liver enzymes.
- Pre-existing Conditions: People with liver conditions like fatty liver disease may see more significant changes in enzyme levels when on TRT.
Changes in Liver Fat Content
Fatty liver disease is a condition where fat builds up in the liver. It can lead to inflammation and liver damage over time. TRT can affect liver fat content in different ways.
TRT and Fat Accumulation:
- Potential Increase in Fat: Some studies suggest that TRT can increase liver fat content, especially in individuals predisposed to fatty liver disease. This is a concern because excess fat in the liver can lead to non-alcoholic fatty liver disease (NAFLD).
- Fat Distribution: TRT can change how the body stores fat. While it might reduce fat in some areas, it can lead to an increase in liver fat. This effect varies among individuals.
Factors Influencing Fat Changes:
- Dosage and Duration: Higher doses of TRT and long-term use might have a more pronounced effect on liver fat content. It's crucial to follow prescribed doses and have regular check-ups.
- Lifestyle Factors: Diet, exercise, and alcohol consumption also play significant roles in liver health. Those on TRT should maintain a healthy lifestyle to mitigate any adverse effects on the liver.
Long-Term Liver Health Considerations
Long-term TRT use requires careful consideration of its impact on liver health. While many people use TRT without serious liver issues, potential risks should be monitored.
Monitoring Liver Health:
- Regular Check-Ups: Periodic liver function tests are vital. These tests help detect early signs of liver damage and allow for timely intervention.
- Lifestyle Adjustments: Adopting a liver-friendly lifestyle is crucial. This includes a balanced diet low in processed foods and high in fruits, vegetables, and lean proteins. Regular exercise and avoiding excessive alcohol are also beneficial.
Potential Risks and Management:
- Liver Conditions: Individuals with pre-existing liver conditions should discuss the risks and benefits of TRT with their healthcare provider. They may need more frequent monitoring.
- Medication Interactions: Some medications can interact with TRT, affecting liver function. Always inform your doctor about all the medications and supplements you are taking.
Benefits vs. Risks:
- Symptom Relief vs. Side Effects: TRT can significantly improve symptoms of low testosterone, such as fatigue, depression, and muscle loss. However, these benefits must be weighed against potential liver-related side effects.
- Individualized Treatment: Each person's response to TRT is different. Personalized treatment plans that include regular monitoring and lifestyle modifications can help manage potential risks.
Understanding how TRT affects liver function is key to using this therapy safely and effectively. Regular monitoring, a healthy lifestyle, and open communication with healthcare providers can help manage any risks associated with TRT, ensuring the best possible outcomes for liver health.
Who is at Risk?
Understanding who is at risk for developing fatty liver disease, especially when undergoing Testosterone Replacement Therapy (TRT), is crucial. Identifying high-risk groups, the role of pre-existing conditions, and the importance of monitoring and screening can help prevent and manage this condition effectively.
Identifying High-Risk Groups
Certain groups of people are more likely to develop fatty liver disease when undergoing TRT. These groups include:
- People with Obesity: Obesity is a major risk factor for fatty liver disease. Excess body weight, especially around the abdomen, increases the risk of fat accumulation in the liver. This risk is heightened when combined with TRT, as hormonal changes can influence fat distribution and metabolism.
- Individuals with Type 2 Diabetes: Diabetes can lead to increased fat storage in the liver. People with type 2 diabetes are more likely to develop non-alcoholic fatty liver disease (NAFLD). When these individuals undergo TRT, their risk of fatty liver disease can increase further.
- Those with Metabolic Syndrome: Metabolic syndrome is a cluster of conditions, including high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels. This syndrome significantly raises the risk of fatty liver disease. Adding TRT to this mix can complicate the body's metabolic balance, potentially exacerbating liver fat accumulation.
- Older Adults: As people age, their metabolism changes, and the risk of developing fatty liver disease increases. Older adults undergoing TRT need to be particularly vigilant, as age-related metabolic changes can affect how the body handles both testosterone and liver fat.
Role of Pre-Existing Conditions
Pre-existing health conditions can influence the risk of developing fatty liver disease during TRT. These conditions include:
- Pre-Existing Liver Disease: Individuals who already have liver conditions, such as hepatitis or cirrhosis, are at a higher risk. TRT can add additional stress to an already compromised liver, potentially worsening these conditions.
- Cardiovascular Diseases: Heart disease and related conditions can be linked to fatty liver disease. People with cardiovascular issues may experience changes in blood flow and metabolism that can increase the likelihood of liver fat accumulation when undergoing TRT.
- Hormonal Imbalances: Conditions that affect hormone levels, such as polycystic ovary syndrome (PCOS) in women or hypogonadism in men, can impact liver health. TRT can interact with these hormonal imbalances, potentially leading to an increased risk of fatty liver disease.
Monitoring and Screening Recommendations
Regular monitoring and screening are essential for individuals at risk of developing fatty liver disease while undergoing TRT. Key recommendations include:
- Regular Blood Tests: Blood tests can help monitor liver function by measuring liver enzymes, such as ALT and AST. Elevated levels of these enzymes can indicate liver inflammation or damage, necessitating further investigation and potential adjustments to TRT.
- Imaging Studies: Imaging techniques, such as ultrasound, CT scans, or MRI, can provide detailed pictures of the liver. These images can help detect early signs of fatty liver disease, allowing for timely intervention.
- Lifestyle Assessments: Regular assessments of diet, physical activity, and overall lifestyle are crucial. Healthcare providers should evaluate these factors to provide personalized recommendations that can help mitigate the risk of fatty liver disease.
- Risk Factor Management: Managing risk factors, such as obesity, diabetes, and metabolic syndrome, is essential. This management might involve weight loss programs, dietary changes, exercise regimens, and medications to control blood sugar and cholesterol levels.
- Consultation with Specialists: Individuals undergoing TRT should regularly consult with their healthcare providers, including endocrinologists and hepatologists. These specialists can provide expert guidance on balancing TRT with liver health and managing any emerging issues.
By understanding who is at risk and taking proactive steps to monitor and manage potential complications, individuals undergoing TRT can better protect their liver health. This approach ensures that the benefits of TRT are maximized while minimizing the risk of developing fatty liver disease. Regular communication with healthcare providers, coupled with lifestyle modifications, plays a pivotal role in achieving this balance.
Preventive Measures for Fatty Liver in TRT Patients
Preventing fatty liver disease (FLD) in patients undergoing testosterone replacement therapy (TRT) requires a multifaceted approach. This section will delve into three primary preventive measures: lifestyle modifications, dietary recommendations, and exercise and physical activity. Each of these strategies plays a crucial role in maintaining liver health and overall well-being.
Lifestyle Modifications
Lifestyle changes are the cornerstone of preventing fatty liver disease, especially for those on TRT. Here are some essential lifestyle modifications to consider:
- Avoiding Alcohol and Smoking:
- Alcohol consumption is a significant risk factor for developing fatty liver. Patients on TRT should limit or eliminate alcohol intake to reduce liver strain.
- Smoking is another harmful habit that can exacerbate liver problems. Quitting smoking is beneficial for liver health and overall cardiovascular health.
- Stress Management:
- Chronic stress can negatively impact liver health by increasing inflammation and oxidative stress. Patients should practice stress-reducing techniques such as meditation, deep breathing exercises, yoga, or engaging in hobbies.
- Adequate Sleep:
- Quality sleep is essential for liver regeneration and overall health. Aim for 7-9 hours of uninterrupted sleep per night to support liver function.
- Regular Health Check-Ups:
- Regular visits to healthcare providers for monitoring liver function and overall health are vital. Routine blood tests can help detect any early signs of liver problems, allowing for timely intervention.
Dietary Recommendations
Diet plays a pivotal role in preventing fatty liver disease. The following dietary recommendations can help maintain liver health:
- Balanced Diet:
- A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats supports liver health. Avoid processed foods, sugary snacks, and high-fat foods that can contribute to liver fat accumulation.
- Healthy Fats:
- Incorporate healthy fats such as those found in avocados, nuts, seeds, and olive oil. These fats help reduce liver inflammation and improve liver function.
- Low Carbohydrate Intake:
- High carbohydrate intake, especially refined carbs, can lead to fat buildup in the liver. Opt for complex carbohydrates like whole grains, which are digested slowly and do not spike blood sugar levels.
- Moderate Protein Intake:
- Adequate protein intake is crucial for liver repair and regeneration. Include lean protein sources such as chicken, fish, legumes, and tofu in your diet.
- Hydration:
- Staying hydrated is essential for liver detoxification. Aim to drink at least 8-10 glasses of water daily to support liver function and overall health.
- Antioxidant-Rich Foods:
- Foods rich in antioxidants, such as berries, leafy greens, and nuts, help protect the liver from oxidative stress and inflammation.
- Avoiding Toxins:
- Limit exposure to environmental toxins and chemicals that can harm the liver. This includes avoiding processed foods with artificial additives and preservatives.
Exercise and Physical Activity
Regular physical activity is one of the most effective ways to prevent fatty liver disease. Here’s how exercise contributes to liver health:
- Weight Management:
- Maintaining a healthy weight is crucial for preventing fatty liver. Obesity is a significant risk factor for fatty liver disease, and regular exercise helps control body weight.
- Fat Reduction:
- Physical activity helps reduce visceral fat, the harmful fat that accumulates around the organs, including the liver. This fat is closely linked to fatty liver disease.
- Improved Insulin Sensitivity:
- Regular exercise enhances insulin sensitivity, which helps regulate blood sugar levels and reduces the risk of fat accumulation in the liver.
- Types of Exercise:
- Incorporate a mix of aerobic exercises (such as walking, running, and swimming) and strength training exercises (such as weightlifting and resistance band exercises) into your routine. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, combined with muscle-strengthening activities on two or more days a week.
- Consistency:
- Consistency is key to reaping the benefits of exercise. Establish a regular exercise routine that fits your lifestyle and stick to it. Even small amounts of physical activity can be beneficial if done regularly.
Preventing fatty liver disease in TRT patients requires a holistic approach that includes lifestyle modifications, dietary changes, and regular physical activity. By making these changes, patients can support their liver health, improve their overall well-being, and enhance the effectiveness of their TRT regimen.
Treatment Strategies for Fatty Liver
Fatty liver disease, also known as hepatic steatosis, occurs when excess fat builds up in the liver. This can lead to liver damage and other serious health problems. For patients undergoing Testosterone Replacement Therapy (TRT), managing and treating fatty liver is crucial. Here are some effective treatment strategies:
Medical Interventions
Medications and Supplements:
For patients with fatty liver, certain medications can help reduce liver fat and improve liver function. Pioglitazone, a drug used to treat diabetes, has been shown to reduce liver fat in patients with non-alcoholic fatty liver disease (NAFLD). Vitamin E supplements can also be beneficial for people with NAFLD, especially for those who do not have diabetes. These medications should always be taken under the supervision of a healthcare provider.
TRT Dosage Adjustments:
It's important to work with a doctor to adjust TRT dosages carefully. High levels of testosterone can sometimes contribute to liver problems. Regular monitoring and appropriate dosage adjustments can help minimize the risk.
Regular Monitoring:
Patients on TRT should have their liver function tested regularly. Blood tests can check for liver enzymes, which indicate how well the liver is working. Imaging tests like ultrasounds or MRIs can also be used to monitor liver fat content. Regular check-ups allow for early detection and treatment of any liver issues.
Role of Medications
Metformin:
This medication is commonly used to manage blood sugar levels in patients with type 2 diabetes. It can also help reduce liver fat in patients with NAFLD. Metformin improves insulin sensitivity and reduces liver fat accumulation.
Statins:
These cholesterol-lowering drugs can also benefit patients with fatty liver. Statins help lower bad cholesterol (LDL) levels and reduce inflammation, which can improve liver health. Patients with both high cholesterol and fatty liver may benefit from statin therapy.
Omega-3 Fatty Acids:
These are found in fish oil supplements and have been shown to reduce liver fat and inflammation. Omega-3 fatty acids can help improve liver function and are a safe supplement for most people.
Bariatric Surgery:
In severe cases of fatty liver disease, weight loss surgery may be recommended. Bariatric surgery can lead to significant weight loss and improvement in liver health. It is usually considered when other treatments have not been successful.
Importance of Regular Monitoring
Blood Tests:
Regular blood tests are essential for monitoring liver health. Tests like ALT (alanine aminotransferase) and AST (aspartate aminotransferase) measure liver enzymes. High levels of these enzymes can indicate liver damage. Regular monitoring helps in early detection and management of liver issues.
Imaging Tests:
Imaging tests like ultrasounds, CT scans, or MRIs provide a clear picture of the liver's fat content. These tests can help monitor the progression of fatty liver disease and the effectiveness of treatment strategies.
Liver Biopsy:
In some cases, a liver biopsy may be necessary. This involves taking a small sample of liver tissue for examination under a microscope. It provides detailed information about the extent of liver damage and inflammation. A biopsy is usually considered when other tests do not provide enough information.
Lifestyle Modifications:
Lifestyle changes are crucial in managing and treating fatty liver disease. These changes can significantly improve liver health and overall well-being.
Dietary Recommendations:
A healthy diet is essential for managing fatty liver. Patients should focus on eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Reducing sugar and saturated fats intake is also important. Avoiding alcohol can help prevent further liver damage.
Exercise and Physical Activity:
Regular physical activity helps reduce liver fat and improve liver function. Patients should aim for at least 150 minutes of moderate-intensity exercise per week. Activities like walking, cycling, and swimming are excellent choices. Strength training exercises can also help improve muscle mass and metabolism.
Weight Management:
Maintaining a healthy weight is crucial for liver health. Even a small amount of weight loss can reduce liver fat and improve liver function. Patients should work with healthcare providers to develop a safe and effective weight loss plan.
Avoiding Toxins:
Patients should avoid exposure to toxins that can harm the liver. This includes limiting the use of certain medications and avoiding alcohol and illicit drugs.
Managing fatty liver disease in TRT patients involves a combination of medical interventions, medications, regular monitoring, and lifestyle changes. By following these strategies, patients can improve their liver health and overall well-being. Regular check-ups and communication with healthcare providers are essential for effective management of fatty liver disease.
Managing TRT While Dealing with Fatty Liver
Testosterone Replacement Therapy (TRT) can be a helpful treatment for men with low testosterone levels. However, managing TRT when you have fatty liver disease can be challenging. It's important to carefully balance the benefits of TRT with the potential risks to your liver health. This section will cover how to adjust TRT dosages, the importance of coordinated care with healthcare providers, and the need for patient education.
Adjusting TRT Dosages
When you have fatty liver disease and are undergoing TRT, it's crucial to monitor your testosterone levels and liver function regularly. Here are some key points to consider:
- Regular Blood Tests: Regular blood tests can help track your testosterone levels and liver enzymes. This allows your doctor to adjust your TRT dosage as needed. Keeping your testosterone levels within the normal range can help minimize the impact on your liver.
- Start with Low Doses: If you are starting TRT and have fatty liver disease, your doctor may recommend starting with a lower dose of testosterone. This approach allows your body to adjust slowly and reduces the strain on your liver.
- Gradual Increases: If your doctor decides to increase your dosage, it should be done gradually. Sudden increases can stress your liver and lead to complications. Your doctor will monitor your progress and adjust your dosage based on your body's response.
Coordinated Care with Healthcare Providers
Managing TRT while dealing with fatty liver disease requires a team approach. Working closely with your healthcare providers is essential. Here’s how you can achieve coordinated care:
- Primary Care Physician (PCP): Your PCP should be aware of your TRT treatment and your fatty liver condition. They can help coordinate care and ensure that both conditions are managed effectively.
- Endocrinologist: An endocrinologist specializes in hormone-related issues. They can provide expert advice on managing your TRT, especially if adjustments to your treatment plan are needed.
- Hepatologist: A hepatologist specializes in liver diseases. They can offer guidance on managing fatty liver disease and work with your endocrinologist to ensure your TRT does not worsen your liver condition.
- Nutritionist: A nutritionist can help you develop a diet plan that supports liver health and complements your TRT. They can advise on foods to include and avoid, ensuring you get the nutrients you need without harming your liver.
Importance of Patient Education
Understanding your treatment and how to manage it is crucial. Here are ways to ensure you are well-informed:
- Educational Materials: Ask your healthcare providers for educational materials about TRT and fatty liver disease. These materials can help you understand the conditions and how they interact.
- Ask Questions: Never hesitate to ask questions during your appointments. Understanding why certain tests are done, what your results mean, and how adjustments to your treatment affect you can help you feel more in control of your health.
- Lifestyle Changes: Learn about lifestyle changes that can benefit both your TRT and fatty liver disease. This includes dietary changes, exercise routines, and avoiding alcohol. A healthy lifestyle can improve your overall health and support your treatment.
- Medication Management: Understand how to take your medications correctly. If you have other medications for fatty liver disease, know how they interact with TRT. This can prevent potential complications.
Detailed Explanation of Points
Regular Blood Tests: Blood tests are essential for monitoring your health. They can detect changes in liver enzymes that may indicate liver stress or damage. By regularly checking your testosterone levels, your doctor can ensure your TRT is effective without harming your liver.
Start with Low Doses: Starting with a lower dose of testosterone reduces the risk of overwhelming your liver. It allows your body to adapt to the new hormone levels gradually. This approach is safer and helps prevent complications.
Gradual Increases: Gradual dosage increases allow your liver to adapt without being overburdened. Rapid changes can lead to liver stress and exacerbate fatty liver disease. Careful monitoring ensures any increase is safe and beneficial.
Coordinated Care: Coordinated care involves multiple healthcare providers working together. Your PCP oversees your general health, while specialists like endocrinologists and hepatologists provide focused care. A nutritionist ensures your diet supports your treatment. This team approach ensures comprehensive care and better health outcomes.
Educational Materials: These materials provide information on your conditions and treatment options. They can include brochures, websites, and instructional videos. Being informed helps you make better health decisions.
Ask Questions: Engaging with your healthcare providers through questions ensures you understand your treatment. It helps build a collaborative relationship where you actively participate in your health management.
Lifestyle Changes: Implementing lifestyle changes like a balanced diet, regular exercise, and avoiding alcohol can significantly improve your liver health and support your TRT. These changes contribute to overall well-being and enhance the effectiveness of your treatment.
Medication Management: Understanding how to take your medications correctly ensures their effectiveness and prevents adverse interactions. Knowing which medications can be taken together and which should be avoided is crucial for managing multiple conditions.
Managing TRT while dealing with fatty liver disease requires careful monitoring and a coordinated approach. Adjusting TRT dosages, ensuring coordinated care with healthcare providers, and prioritizing patient education are key to successful management. By staying informed and proactive, you can achieve better health outcomes and effectively manage both conditions.
Future Directions and Research
Understanding the relationship between Testosterone Replacement Therapy (TRT) and fatty liver disease is crucial. As we learn more, we can improve treatments and outcomes for patients. This section looks at the future directions and research in this field. We will discuss emerging studies, potential new therapies, and the importance of ongoing research.
Emerging Studies on TRT and Liver Health
Researchers are continually studying how TRT affects liver health. New studies are helping us understand the connection between testosterone levels and liver function. These studies focus on several key areas:
Hormonal Impact: Scientists are exploring how testosterone influences liver enzymes and metabolism. They are examining whether testosterone helps or harms liver cells. Understanding this hormonal impact is essential for determining the safety and effectiveness of TRT.
Long-term Effects: Long-term studies are being conducted to observe the effects of TRT over many years. These studies track patients receiving TRT to see how their liver health changes over time. This information helps doctors predict the risks and benefits of TRT for long-term users.
Population Studies: Researchers are also looking at different populations, including men with different health conditions. For example, studies focus on men with pre-existing liver diseases, diabetes, and obesity. These studies help identify which groups may be more at risk and require special attention.
Potential New Therapies
As we learn more about TRT and liver health, new therapies are being developed. These potential new therapies aim to provide better treatment options for patients. Here are some promising areas of development:
Improved TRT Formulations: Scientists are working on new formulations of testosterone that are safer and more effective. These formulations aim to deliver testosterone in a way that minimizes risks to the liver. For example, new methods of delivering testosterone, such as patches or gels, might reduce liver strain compared to oral medications.
Combination Therapies: Another area of research is the use of combination therapies. Researchers are exploring whether combining TRT with other medications can improve outcomes. For instance, combining TRT with drugs that protect the liver or improve metabolism might enhance treatment effectiveness while reducing risks.
Gene Therapy: Gene therapy is an exciting field that holds promise for future treatments. Scientists are investigating whether modifying certain genes can help regulate testosterone levels and improve liver health. While still in the experimental stage, gene therapy could offer a revolutionary approach to managing conditions like fatty liver disease.
Importance of Ongoing Research
Ongoing research is vital for advancing our understanding and treatment of TRT and fatty liver disease. Here’s why continuous research is so important:
Addressing Knowledge Gaps: There are still many unknowns about how TRT affects the liver. Ongoing research helps fill these gaps in knowledge. For example, researchers are studying why some men develop liver issues on TRT while others do not. Understanding these differences can lead to more personalized treatments.
Improving Patient Outcomes: Research aims to improve the outcomes for patients receiving TRT. By studying different treatment approaches and patient responses, scientists can develop better guidelines for doctors. This ensures that patients receive the most effective and safest care possible.
Guiding Clinical Practice: New research findings guide clinical practice. Doctors rely on up-to-date research to make informed decisions about prescribing TRT. As new information becomes available, treatment protocols are updated to reflect the latest evidence.
Advancing Public Health: Beyond individual patient care, ongoing research has broader public health implications. Understanding the impact of TRT on liver health can inform public health policies and recommendations. This helps protect the health of the wider population and ensures that TRT is used safely and effectively.
The future of TRT and fatty liver disease research is promising. Emerging studies, new therapies, and the continuous pursuit of knowledge are all critical for improving patient care. As research progresses, we can look forward to safer and more effective treatments, ultimately enhancing the quality of life for those affected by these conditions.
Conclusion
In this comprehensive guide, we explored the complex relationship between Testosterone Replacement Therapy (TRT) and fatty liver disease. Understanding this connection is crucial for those undergoing TRT or considering it, especially if they are at risk for or already have fatty liver disease.
First, we discussed the basics of TRT. Testosterone Replacement Therapy is a treatment used to increase testosterone levels in men with low testosterone. It can help with symptoms like fatigue, mood swings, and decreased libido. TRT is available in several forms, including injections, patches, gels, and pellets.
Next, we delved into fatty liver disease, which can be either non-alcoholic (NAFLD) or alcoholic (AFLD). NAFLD is more common and is often linked to obesity, diabetes, and high cholesterol. Fatty liver disease occurs when too much fat builds up in liver cells. This can lead to inflammation and, over time, serious liver damage.
The link between TRT and fatty liver disease is a topic of ongoing research. Testosterone can affect liver metabolism, and studies have shown mixed results. Some research suggests that TRT might help reduce liver fat and improve liver health in men with low testosterone. However, other studies indicate potential risks, such as liver enzyme changes. It is crucial to balance these risks and benefits when considering TRT.
TRT can affect liver function in various ways. It may alter liver enzyme levels, which are used to measure liver health. Some people on TRT might see an increase in these enzymes, indicating liver stress. However, TRT can also reduce liver fat in some cases, potentially benefiting those with fatty liver disease. Long-term effects on liver health are still not fully understood and need careful monitoring.
Certain groups are at higher risk of developing fatty liver disease while on TRT. These include individuals with obesity, diabetes, high cholesterol, or existing liver conditions. Screening and regular monitoring are essential for these high-risk groups. This helps in catching any adverse effects early and managing them effectively.
Preventing fatty liver disease in those undergoing TRT involves lifestyle changes. A healthy diet is crucial. Reducing sugar and fat intake, eating more fruits and vegetables, and avoiding alcohol can help. Regular exercise is also important as it helps maintain a healthy weight and reduces liver fat. These lifestyle changes support liver health and overall well-being.
Treatment strategies for fatty liver disease include medical interventions and medications. Doctors may prescribe drugs to manage conditions that contribute to fatty liver, such as diabetes or high cholesterol. Regular check-ups and liver function tests are important to monitor the liver's health and the effectiveness of the treatment.
Managing TRT while dealing with fatty liver disease requires a coordinated approach. Healthcare providers need to adjust TRT dosages carefully and monitor liver function regularly. Patients should be educated about the potential risks and benefits of TRT and the importance of adhering to prescribed treatments and lifestyle recommendations. This collaborative approach helps in managing both low testosterone and liver health effectively.
Future research is vital in understanding the long-term effects of TRT on liver health. Emerging studies are exploring new therapies and treatment strategies. Ongoing research will help clarify the benefits and risks of TRT for individuals with fatty liver disease. Staying informed about the latest findings is important for healthcare providers and patients alike.
In summary, the relationship between TRT and fatty liver disease is complex and requires careful consideration. While TRT can offer significant benefits for men with low testosterone, it is essential to monitor liver health closely. Lifestyle changes, regular monitoring, and a collaborative approach with healthcare providers are key to managing both TRT and fatty liver disease effectively. By staying informed and proactive, individuals can make better decisions about their health and treatment options. This guide aims to provide a thorough understanding of the connection between TRT and fatty liver disease, empowering readers to take charge of their health with confidence.
Questions and Answers
TRT is a medical treatment used to increase testosterone levels in men who have low levels due to various conditions, including hypogonadism.
Fatty liver disease, also known as hepatic steatosis, is a condition where excess fat builds up in the liver. It can be caused by alcohol (alcoholic fatty liver disease) or other factors (non-alcoholic fatty liver disease).
TRT has the potential to impact liver health, though studies show mixed results. Some research indicates TRT may benefit liver function, while other studies suggest potential risks, particularly in individuals with pre-existing liver conditions.
Fatty liver disease can lead to liver inflammation, fibrosis, cirrhosis, and in severe cases, liver failure. It is also associated with an increased risk of cardiovascular diseases and type 2 diabetes.
Yes, low testosterone levels have been linked to an increased risk of developing non-alcoholic fatty liver disease (NAFLD) due to insulin resistance and metabolic syndrome, conditions that are also associated with low testosterone.
Some studies suggest TRT may improve metabolic health and reduce liver fat in men with low testosterone and NAFLD. However, further research is needed to establish definitive benefits and risks.
Potential side effects of TRT include increased red blood cell count, acne, sleep apnea, prostate growth, and potential cardiovascular risks. Liver toxicity is a rare but possible side effect.
Fatty liver disease is typically diagnosed through imaging tests such as ultrasound, CT scan, or MRI. Blood tests and liver biopsies may also be used to assess liver function and fat content.
Lifestyle changes such as weight loss, healthy eating, regular physical activity, reducing alcohol consumption, and managing diabetes and cholesterol can help manage and potentially reverse fatty liver disease.
Individuals with fatty liver disease should consult with a healthcare provider before considering TRT. A thorough evaluation of the potential benefits and risks based on their overall health and liver condition is essential.