HRT for Extreme Hot Flashes Treatment
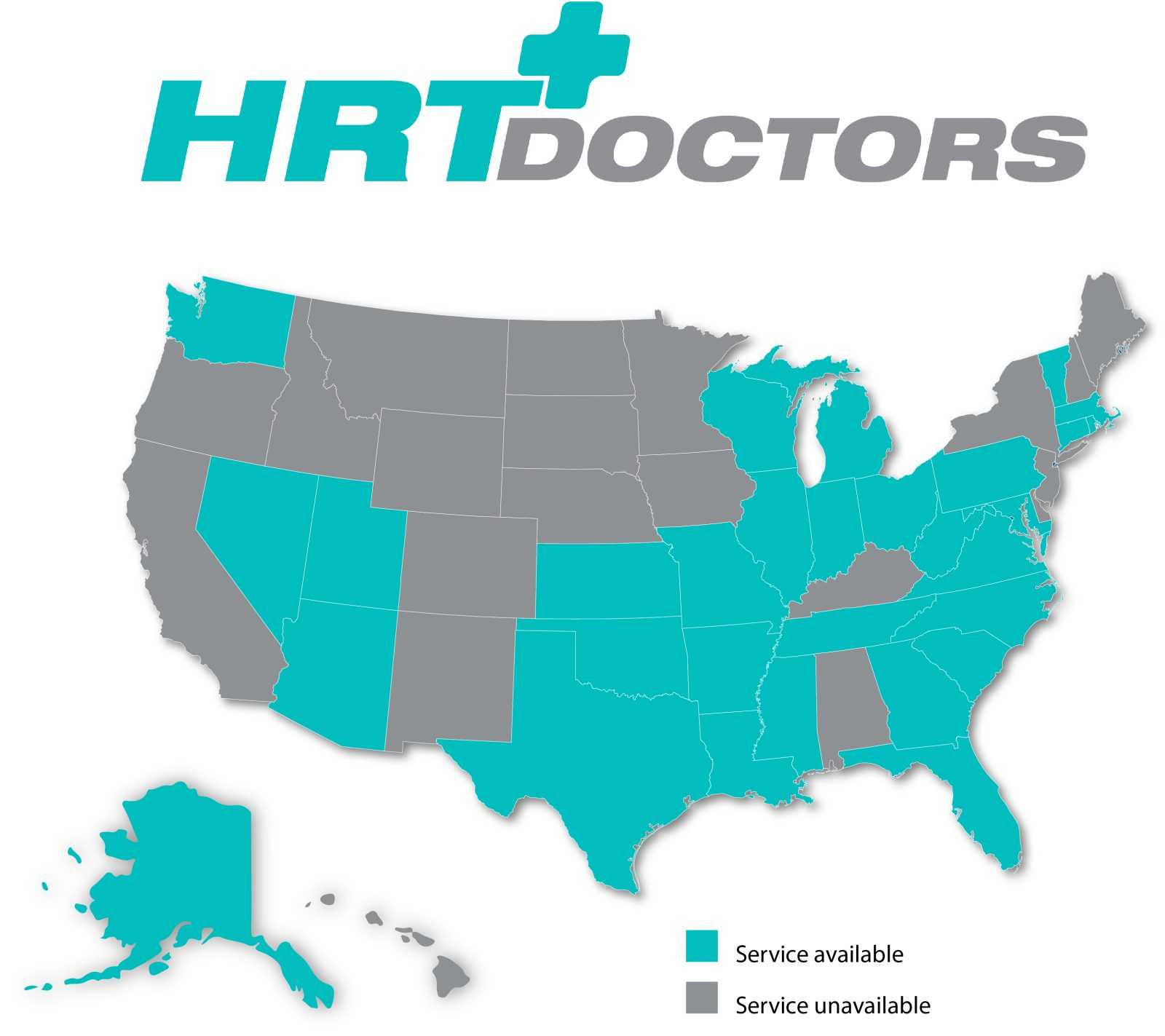
HRT Doctors is a nationwide telemedicine clinical practice specializing in Hormone Replacement Therapy (HRT) for patients seeking treatment for extreme hot flashes.
Hormonal imbalance symptoms & extreme hot flashes can be debilitating and may sometimes reflect an underlying endocrine condition. You can click here to learn more about hormone related symptoms.
Our board-certified HRT doctors use Telemedicine to give convenient and more affordable access to Quality Care.
Our clinical practice can provide guidance to new patients seeking hormone therapy options or existing patients that are simply looking to switch to a more convenient telemedicine-based practice.
As Seen On

Board Certified HRT Doctors Available In 31 States Nationwide.
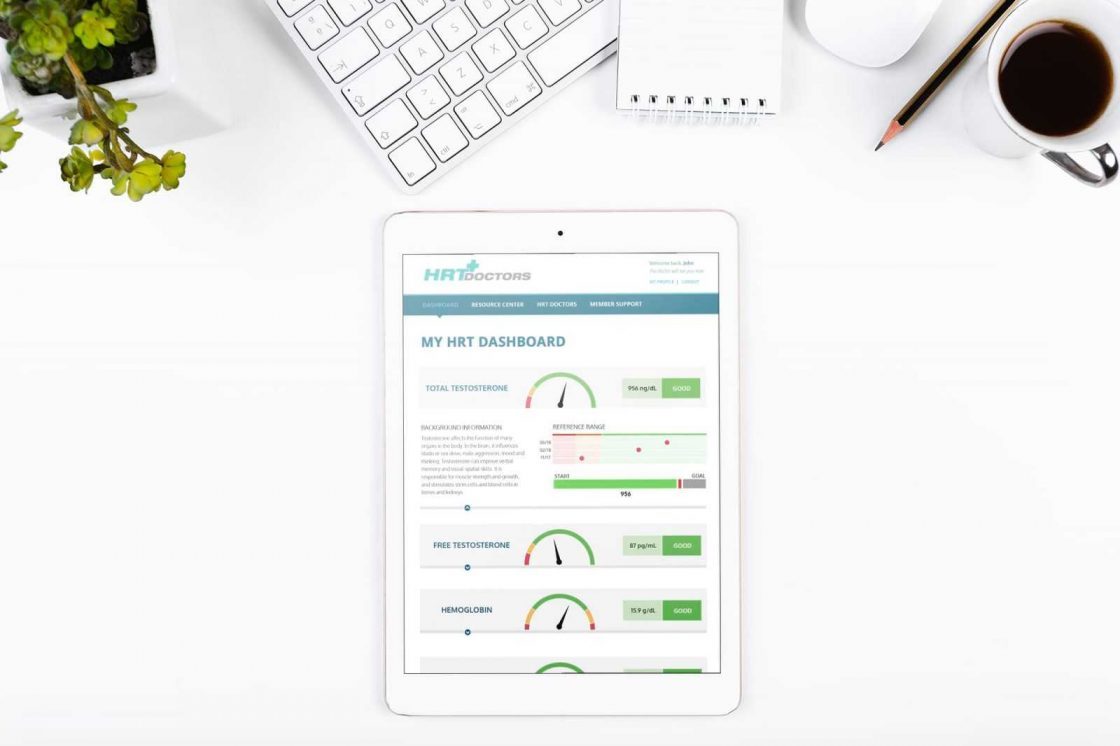
We have partnered with the nationwide laboratory, Quest Diagnostics, to provide accurate lab blood work testing and results. Lab processing time typically takes 5 to 6 business days.
HRT Dashboard
How The HRT Program Works
01
Complete Clinical Services Checkout For $89.95
This clinical services set-up fee covers your initial electronic medical record review, Quest Diagnostics laboratory services to determine your current hormone levels and other key wellness attributes, and your first virtual doctor’s visit.
02
Complete Your Medical History
Provide our Board-Certified HRT Doctor’s with your medical history via our HIPAA-compliant platform.
03
Complete Your Labs
We have partnered with the nationwide laboratory, Quest Diagnostics, to provide accurate lab testing and results. You can complete your blood test at any Quest Diagnostics nearby.
04
Consult With Our Doctors
Our Board Certified HRT Doctors use telemedicine to give convenient and more affordable access to quality care. Our HRT physicians will consult with you to review your lab results, and discuss any current complaints, conditions, and symptoms . Based on the results of your consultation, the HRT Wellness physician will recommend the best treatment options.
05
Home Treatment & Continued Patient Care
Your treatment prescriptions will be shipped directly to you. Our Patient Care Team will provide in-depth assistance as you begin and progress through your treatment plan.