Low T Lymphocytes Uncovered: What Happens When Your Immune Army Shrinks
Introduction: Understanding the Immune Army
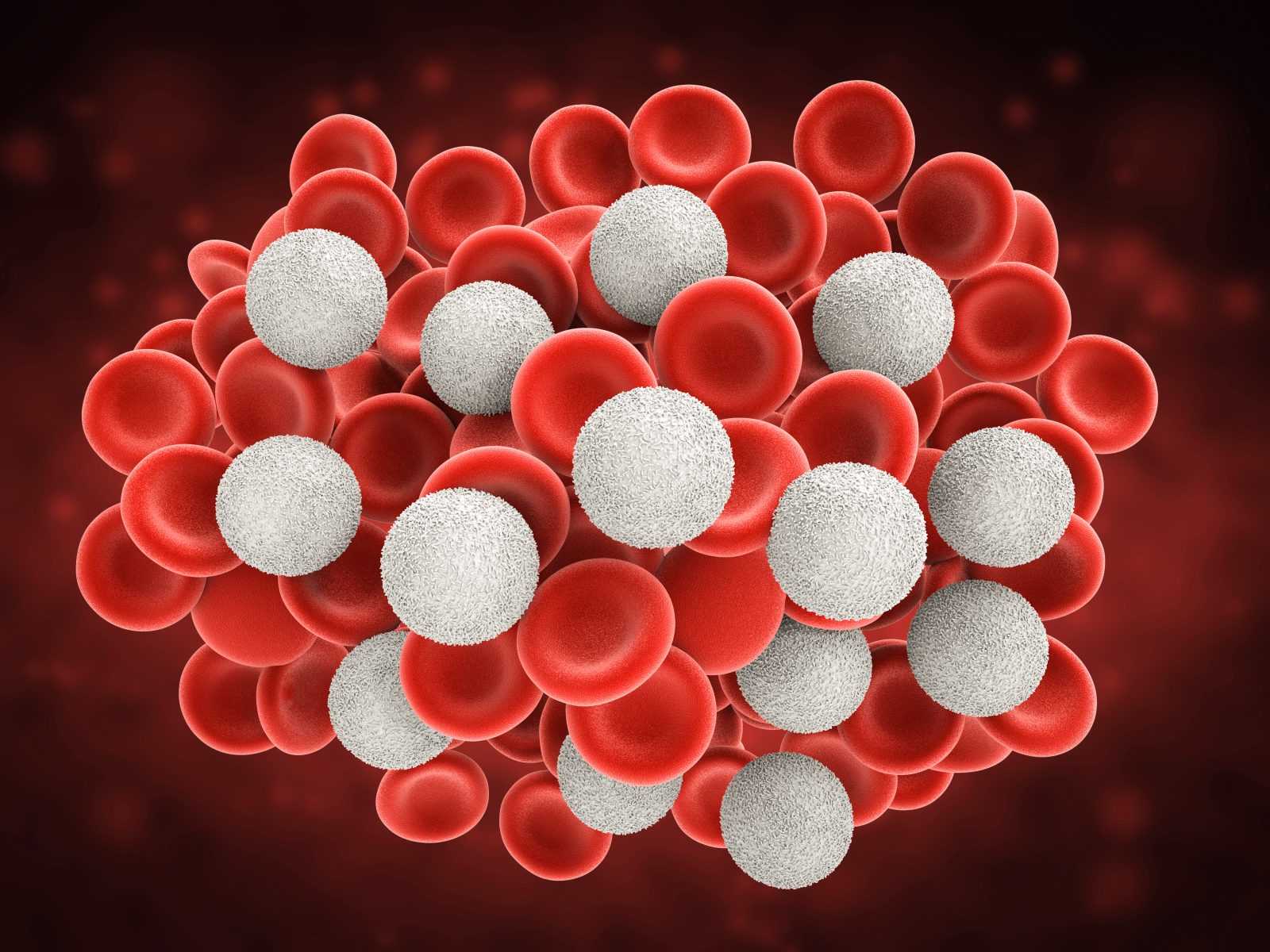
The human body has a natural defense system called the immune system. This system protects the body from infections, viruses, and other harmful substances. One of the most important parts of the immune system is a group of white blood cells called lymphocytes. These cells help the body recognize and fight off harmful invaders. There are two main types of lymphocytes: B cells and T cells. While both are important, T lymphocytes, or T cells, have a unique and powerful role in protecting health.
T cells come from the bone marrow but mature in an organ called the thymus. Once they are fully developed, they move through the body in the blood and lymph system. They search for signs of infection or abnormal cells. T cells do not make antibodies like B cells. Instead, they help by either killing infected cells directly or by sending signals that guide other immune cells.
There are different types of T cells. The two main types are CD4+ T cells, also known as helper T cells, and CD8+ T cells, also known as cytotoxic T cells. Helper T cells tell other cells in the immune system what to do. They help B cells make antibodies and guide other white blood cells to the infection. Cytotoxic T cells, on the other hand, attack and destroy cells that are infected with viruses or that have become cancerous.
The number of T cells in the blood is a good sign of how strong the immune system is. When the number of T cells drops too low, the immune system becomes weak. This makes it harder for the body to fight infections and diseases. A low T cell count is called lymphocytopenia. People with low T cells may get sick more often, take longer to heal, or have unusual infections.
There are many reasons why T cells might drop below normal levels. Some causes are temporary, like a common viral infection. Others are more serious, like cancer treatments, autoimmune diseases, or HIV infection. Sometimes, people are born with problems in their immune system that lead to low T cell levels. Doctors use blood tests to measure the number of T cells and check which types are low.
Understanding how T cells work and what happens when their numbers drop is important for recognizing immune system problems early. When the body does not have enough T cells, it is like an army with too few soldiers. The defenses become weak, and the body is at greater risk of attack.
In recent years, interest in T lymphocytes has grown due to their role in diseases like HIV, cancer, COVID-19, and autoimmune disorders. Scientists are also studying how T cells can be used in new treatments, such as cancer immunotherapy. These treatments help the body’s own immune system fight cancer by boosting T cell activity.
People often search for answers about low T lymphocytes online, trying to understand what it means for their health or the health of someone they care about. Common questions include what causes low T cells, how they are tested, what symptoms to look for, and whether the levels can return to normal. There is also concern about how lifestyle factors like stress, sleep, and diet can affect the immune system and T cells.
This article explores all of these important questions. It explains what T lymphocytes are, how they function, why their levels may drop, and what effects this can have on the body. It also describes how doctors diagnose and treat low T cell counts, and what steps might help support immune health. Understanding the role of T cells is a key part of staying informed and staying healthy. When the immune army shrinks, it’s vital to know what is happening and what can be done.
What Are T Lymphocytes and Why Are They Important?
T lymphocytes, also called T cells, are a type of white blood cell. These cells are a key part of the immune system. The immune system is the body’s defense system. It protects against germs like viruses, bacteria, and other harmful invaders. T cells help the immune system find and fight these invaders.
T cells are made in the bone marrow, which is the soft tissue inside bones. After they are made, they move to the thymus. The thymus is a small organ in the chest where T cells learn how to do their job. That is why they are called “T” cells—because they mature in the thymus.
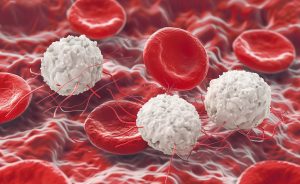
There are several types of T cells. Each type has its own special job. The two main types are helper T cells and cytotoxic T cells. Helper T cells are also called CD4 cells. Cytotoxic T cells are also called CD8 cells.
Helper T Cells (CD4)
Helper T cells are like generals in the immune army. They do not fight germs directly, but they tell other immune cells what to do. When a germ enters the body, helper T cells give signals to other immune cells, like B cells and cytotoxic T cells. These signals help the other cells make antibodies or kill infected cells.
Helper T cells also help start the immune response. Without them, the immune system cannot work well. A low number of CD4 cells can lead to weak immune defense. People with low CD4 cells may get sick more often and take longer to get better.
Cytotoxic T Cells (CD8)
Cytotoxic T cells are the killers of the immune system. Their job is to find and destroy infected cells. When a virus or bacteria enters a cell, that cell becomes a threat. CD8 T cells recognize these infected cells and destroy them before the infection can spread.
These T cells also play a role in cancer defense. They can sometimes detect and destroy cancer cells. If CD8 cells are too low, the body may have a harder time fighting infections and cancer.
Regulatory and Memory T Cells
Other types of T cells include regulatory T cells and memory T cells.
Regulatory T cells help keep the immune system in balance. They stop the immune system from attacking healthy cells. This is important because sometimes the immune system can make a mistake and attack the body’s own tissues. That mistake can lead to diseases like lupus or rheumatoid arthritis.
Memory T cells help the body remember past infections. After fighting off an infection, some T cells become memory cells. These cells stay in the body for a long time. If the same germ tries to infect the body again, memory T cells help respond faster and stronger. This is how vaccines work—they train the body to make memory T cells against certain diseases.
T Cells vs. B Cells and NK Cells
T cells are one part of the immune system. Other important cells include B cells and natural killer (NK) cells.
B cells make antibodies. Antibodies are proteins that stick to germs and mark them for destruction. B cells work closely with helper T cells. T cells help B cells know which antibodies to make.
NK cells are part of the body’s first line of defense. They attack infected or cancerous cells without needing to recognize a specific threat. T cells are more targeted and take longer to respond, but they are stronger and more specific.
Why T Cells Are So Important
T cells are vital for health. They help the body fight infections, destroy abnormal cells, and keep the immune system working the right way. If T cell levels drop too low, the immune system becomes weak. This can lead to frequent infections, slower healing, and more risk of serious illness. Keeping T cells at healthy levels is key to staying well.
What Causes Low T Lymphocyte Counts (Lymphocytopenia)?
T lymphocytes, also known as T cells, are a type of white blood cell that help the immune system fight infections and diseases. When the number of these cells drops too low, the condition is called lymphocytopenia. There are many reasons why someone may have low T lymphocyte levels. Some causes are present at birth, while others develop later in life.
Primary Causes: Problems Present from Birth
Some people are born with conditions that affect the development or function of their immune system. These are called primary immunodeficiencies. In these cases, the body has trouble making enough healthy T cells, or the T cells do not work correctly.
One example is DiGeorge syndrome, a disorder where part of the thymus gland is missing or underdeveloped. The thymus is an organ that helps young T cells grow and learn how to fight germs. Without a working thymus, T cells cannot mature properly.
Another rare condition is Severe Combined Immunodeficiency (SCID). Babies born with SCID have very few or no T cells. This makes them extremely vulnerable to infections. These conditions often need early treatment, such as bone marrow transplants, to help restore immune function.
Secondary Causes: Factors That Develop Over Time
In most people, low T cell counts are not caused by genetic conditions. Instead, they are caused by other health problems or outside factors. These are known as secondary causes. They include infections, medicines, autoimmune diseases, poor nutrition, stress, and aging.
Viral Infections
Some viruses directly attack the immune system and lower T cell numbers. The most well-known example is HIV (Human Immunodeficiency Virus). HIV infects and destroys CD4+ T cells, a type of helper T cell. Over time, this leads to a weakened immune system, making it harder for the body to fight infections.
Other viruses, such as Epstein-Barr virus (EBV), cytomegalovirus (CMV), and SARS-CoV-2 (the virus that causes COVID-19), can also temporarily lower T cell counts. In some cases, these changes are short-term and improve as the body recovers. However, if the infection is severe or long-lasting, the drop in T cells can be more serious.
Medications and Treatments
Some medical treatments can damage or lower the number of T cells. For example, chemotherapy and radiation therapy used for cancer can harm the bone marrow, where immune cells are made. This reduces the production of new T cells.
Immunosuppressive medications, often given to people with autoimmune diseases or after organ transplants, can also lower T cell levels. These drugs are used to calm the immune system but may also weaken its ability to protect the body from infections.
Autoimmune Diseases
In autoimmune diseases, the immune system mistakenly attacks the body’s own tissues. This confusion can also lead to problems with immune cell counts. Conditions like lupus and rheumatoid arthritis can affect how T cells are made or how they survive in the body. The inflammation from these diseases may also cause T cells to die faster than normal.
Malnutrition and Poor Diet
A healthy immune system needs proper nutrition. When the body does not get enough nutrients, it cannot make enough white blood cells, including T cells. Protein-energy malnutrition is especially harmful because proteins are needed to build immune cells. Deficiencies in zinc, iron, vitamin A, and other nutrients can also lead to low T cell counts.
Physical and Emotional Stress
Chronic stress has a direct impact on the immune system. When the body is under constant stress, it produces high levels of a hormone called cortisol. Cortisol helps the body respond to stress, but in large amounts, it can suppress T cell activity and even lead to their breakdown. Long-term emotional stress, trauma, or lack of sleep can all contribute to lower T cell counts over time.
Aging
As people get older, their immune system naturally becomes weaker. The thymus gland, where T cells mature, shrinks with age. This leads to fewer new T cells being made. Older adults also tend to have fewer naïve T cells—the ones that can recognize new infections. Instead, they have more memory T cells that are programmed to fight past infections, which may not help with new threats.
When T lymphocyte levels fall below the normal range, the immune system becomes less able to defend the body. Whether the cause is present from birth or develops later, understanding the reason behind low T cells is important for choosing the right treatment and protecting overall health.
How Is a Low T Cell Count Diagnosed?
T lymphocytes, or T cells, play a central role in the immune system. When someone has a low T cell count, the body may have a harder time fighting infections and staying healthy. Diagnosing a low T cell count involves looking at symptoms, running certain blood tests, and sometimes doing more advanced testing. Understanding how doctors find out if T cells are low can help explain why some people may feel sick more often or take longer to recover from illness.
Common Symptoms That Lead to Testing
A low T cell count may not always cause clear symptoms at first. But over time, it can lead to more frequent or severe infections. These may include colds, flu, or other viruses that last longer than usual. Some people may also get sick from bacteria or fungi that normally do not cause illness in healthy people. Skin rashes, fever that won't go away, weight loss, or feeling tired all the time can also be signs that the immune system is weak. When these symptoms appear, doctors may begin testing the blood to look at the immune system.
Blood Tests: The First Step
One of the main ways to check for low T cells is through a blood test. The first test usually done is a Complete Blood Count, or CBC. This test gives basic information about the types of cells in the blood, including white blood cells, red blood cells, and platelets. White blood cells include lymphocytes, which are a group of immune cells that includes T cells.
The CBC can show the total lymphocyte count, which is a useful first clue. If the lymphocyte number is low, the doctor may order more specific tests to look closely at the types of lymphocytes.
Flow Cytometry: Looking at T Cell Types
To understand more about the T cells, doctors often use a test called flow cytometry. This test can measure different types of T cells, like CD4+ helper T cells and CD8+ cytotoxic T cells. These names come from markers on the surface of the cells that help tell them apart.
- CD4+ T cells help other cells in the immune system work properly.
- CD8+ T cells can kill infected or cancerous cells.
Flow cytometry shows how many of each type are in the blood. It also gives the CD4/CD8 ratio, which helps doctors understand the balance between these two types. In healthy people, this ratio is usually between 1.0 and 3.5. A low ratio may mean that CD4+ T cells are especially low, which can be a sign of immune problems.
This test is very useful in conditions like HIV infection, where the CD4+ count is closely watched. But it can also help in many other illnesses, such as autoimmune diseases or after chemotherapy.
Absolute Count vs. Percentage
Doctors may look at both the absolute number of T cells and the percentage they make up in the blood.
- The absolute count tells the exact number of T cells in a certain amount of blood.
- The percentage tells what part of the total lymphocytes are T cells.
Both numbers are important. For example, if a person has a low number of total lymphocytes, even a normal percentage of T cells could still mean that the absolute number of T cells is too low.
When Further Testing Is Needed
Sometimes, blood tests are not enough. If the cause of low T cells is not clear, doctors may need to do more tests. These could include:
- Imaging tests, such as a chest X-ray or CT scan, to check the thymus or look for infections.
- Bone marrow biopsy, where a small sample of bone marrow is taken to check how blood cells are made.
- Blood tests for viruses, such as HIV or Epstein-Barr virus, to see if an infection is lowering the T cell count.
- Genetic testing, in rare cases, if doctors suspect a condition present from birth (congenital immunodeficiency).
These extra tests help find out why the T cells are low and guide decisions about treatment.
Diagnosing a low T cell count takes more than just one test. Doctors look at symptoms, test results, and possible causes. It is important to understand that low T cells are not a disease by themselves but a sign that something may be affecting the immune system. Finding the reason behind the low count helps in planning the best care and protecting the body from more harm.
What Happens to the Body When T Lymphocytes Are Too Low?
T lymphocytes, or T cells, are an important part of the immune system. They help the body fight infections and keep the immune system balanced. When the number of T lymphocytes drops too low, the body has a harder time defending itself. This condition is called lymphocytopenia, and it can cause a variety of health problems.
Greater Risk of Infections
The first and most serious problem caused by low T cells is a higher risk of infections. T cells help the body recognize and destroy viruses, bacteria, and other harmful invaders. Without enough T cells, the immune system becomes weak. This means even mild infections can become more serious or last longer than usual.
People with low T cell counts may get sick more often. They can develop repeated respiratory infections, such as sinus infections, bronchitis, or pneumonia. Some may also experience frequent skin infections, mouth sores, or diarrhea caused by stomach bugs. These infections might not go away easily with regular treatment.
In addition, rare or unusual infections may occur. These are called opportunistic infections. They usually don’t affect people with healthy immune systems, but they can be dangerous for someone with low T cells. For example, fungi like Pneumocystis jirovecii or viruses like cytomegalovirus (CMV) can cause serious illness in people who are immunocompromised.
Weaker Response to Vaccines
T cells also help the body "remember" viruses and bacteria it has seen before. This memory allows the immune system to respond faster the next time it encounters the same germ. Vaccines use this system by teaching the immune system to recognize a virus without causing disease.
When T lymphocyte levels are too low, vaccines may not work well. The body might not create enough memory cells. As a result, vaccinated people may still get the disease the vaccine is supposed to protect them from. This is especially important for vaccines against viruses like influenza, hepatitis B, or COVID-19.
Reactivation of Old Infections
Some infections can stay hidden in the body for many years. These infections are called latent infections. The immune system usually keeps them under control, even if they don’t completely go away. However, when T cells are low, these dormant infections can become active again.
One example is the herpes virus, which can live in nerve cells. It may return as cold sores, shingles, or more serious infections if T cell levels drop. Tuberculosis (TB) is another example. A person may have inactive TB for years, but low immunity can allow the disease to come back and cause symptoms like coughing, fever, and weight loss.
Problems with Immune Balance
T lymphocytes don’t just fight germs. They also help control how the immune system reacts. Some types of T cells stop the immune system from attacking the body’s own cells. When these cells are missing or too low, the immune system may become confused.
This can lead to autoimmune problems, where the immune system starts attacking healthy tissue. Examples include joint pain from rheumatoid arthritis or skin rashes from lupus. These diseases can become worse when the immune system is not balanced.
Low T cells can also make it harder for the immune system to stop inflammation. This can lead to ongoing swelling and damage in parts of the body, such as the lungs, intestines, or nervous system.
Cancer Surveillance Becomes Weaker
T lymphocytes play a quiet but important role in checking the body for abnormal cells. They help recognize cells that might be turning into cancer. If T cell levels are too low, this defense system may not work properly. Over time, this can allow abnormal cells to grow unchecked.
People with long-term lymphocytopenia may have a higher risk for certain types of cancer, especially lymphomas, leukemia, and some virus-related cancers. While this risk depends on many factors, it is one reason why keeping a healthy immune system is so important.
When T lymphocyte levels fall too low, the body loses a key line of defense. This can lead to more infections, poor vaccine response, reactivated illnesses, and loss of immune control. It can also increase the risk of chronic inflammation and some cancers. Understanding these effects helps explain why doctors carefully monitor T cell counts in people with weakened immune systems.
What Is the Difference Between CD4 and CD8 T Cells and Why Does It Matter?
T lymphocytes, or T cells, are a type of white blood cell that play a major role in the immune system. There are two main types of T cells: CD4 T cells and CD8 T cells. These two groups of cells have different jobs, and both are important for protecting the body from disease. When the number of these cells drops too low, the body can struggle to fight infections and other health problems.
CD4 T Cells – The "Helper" Cells
CD4 T cells are often called "helper T cells." These cells help other immune cells do their jobs better. When a harmful germ, such as a virus or bacteria, enters the body, CD4 T cells send signals to alert the rest of the immune system. These signals are special proteins called cytokines. Cytokines help activate other cells, such as B cells and CD8 T cells.
B cells, once activated, can make antibodies to fight the infection. CD8 T cells, which are described below, are better able to destroy infected or cancerous cells when guided by CD4 cells. Without enough CD4 T cells, the immune system becomes weak and slow to respond.
A well-known example of this problem is HIV (Human Immunodeficiency Virus). This virus directly attacks and destroys CD4 T cells. As the number of CD4 cells drops, people with HIV become more likely to get infections that healthy people usually fight off easily. If CD4 levels fall too low, the condition can become AIDS (Acquired Immunodeficiency Syndrome).
CD4 cells also help form immune memory. This means the body can remember how to fight off infections it has seen before. Vaccines work better when there are enough CD4 cells to help build this immune memory.
CD8 T Cells – The "Killer" Cells
CD8 T cells are also known as cytotoxic T cells or "killer T cells." These cells attack and destroy other cells in the body that are infected with viruses or that have turned into cancer cells. They do this by recognizing small pieces of virus or abnormal proteins on the surface of infected cells. Once a target is found, CD8 cells release toxic substances that break apart and kill the sick cell.
CD8 T cells are important for clearing viruses like influenza, hepatitis, and even some types of cancer. If there are not enough CD8 T cells, the body may not be able to clear an infection completely. This could allow the virus to hide inside the body for a long time and possibly come back later.
CD8 cells are also involved in immune surveillance, which means they help keep the body free of cancer by destroying cells that look abnormal. When CD8 levels are low, the chance of certain cancers might increase, especially in people who are already at risk.
CD4/CD8 Ratio and Why It Matters
Doctors often look at both CD4 and CD8 T cell counts in blood tests. These numbers are usually reported as part of a flow cytometry test. A common way to measure immune health is to calculate the CD4/CD8 ratio. This ratio compares the number of helper cells (CD4) to killer cells (CD8).
A healthy CD4/CD8 ratio is usually between 1.0 and 4.0, meaning there are more CD4 cells than CD8 cells. A low ratio (below 1.0) may suggest a weakened immune system. This is often seen in people with HIV, long-term viral infections, or immune aging (also called immunosenescence). A high ratio could happen after a strong immune response or recovery, but it can also mean that CD8 cells are too low.
Tracking the CD4/CD8 ratio helps doctors understand if a person's immune system is balanced or out of order. For example:
- In HIV, a falling CD4 count and a low CD4/CD8 ratio are signs that the virus is winning.
- In some autoimmune diseases, the CD8 level may fall, making the ratio unusually high.
- In elderly people, changes in this ratio can show signs of immune system aging.
Both CD4 and CD8 T cells are essential to immune health. CD4 cells guide and support other immune cells, while CD8 cells attack and destroy infected or dangerous cells. When either of these groups is too low, or when the balance between them is off, the body becomes more vulnerable to infections, cancers, and immune-related diseases.
Understanding these two types of T cells, and keeping track of their levels, helps doctors know how well a person’s immune system is working. It also helps guide treatment in many medical conditions, from infections to cancers to autoimmune problems.
Can Stress or Lifestyle Affect T Lymphocyte Levels?
T lymphocytes, also known as T cells, are a type of white blood cell that helps protect the body from infections and diseases. These cells play a central role in the immune system. While medical conditions and infections can directly lower T cell levels, everyday factors like stress, sleep, diet, and habits also have a strong effect. Even small changes in lifestyle can either support or weaken the immune system.
Stress and the Immune System
Stress is a natural part of life. It can be short-term, like feeling nervous before a test, or long-term, such as ongoing problems at work or home. The body responds to stress by releasing hormones, including cortisol. Cortisol is helpful in small amounts. It helps the body deal with emergencies. But when stress lasts for a long time, cortisol levels stay high.
Long-term high cortisol weakens the immune system. It can reduce the number of T lymphocytes in the blood. It also makes T cells less active, so they don’t work as well in fighting infections. Chronic stress may also lower the number of new T cells made in the bone marrow and thymus, which are the body’s T cell “factories.”
People under long-term stress may get sick more often. They may also take longer to recover from illnesses. This is not just a feeling — it has been shown in studies. For example, caregivers for very sick family members often show lower T cell activity compared to others.
The Role of Sleep
Sleep is vital for good health. During sleep, the body rests and repairs itself. The immune system also uses this time to reset and rebuild. T cells become more active while the body sleeps. Some sleep-related hormones, such as melatonin, support the immune system and help T cells do their job.
Lack of sleep, especially over several nights, can lower T cell numbers. It can also reduce their ability to find and kill virus-infected cells. People who sleep fewer than six hours a night for long periods may be more likely to get colds, the flu, or other infections.
Getting enough sleep — at least 7 to 9 hours per night for most adults — helps the immune system stay strong.
Exercise and T Lymphocytes
Regular exercise supports a healthy immune system. Moderate activity, such as walking, swimming, or biking for 30 minutes most days, can improve T cell function. It helps increase blood flow, which helps T cells move around the body more easily. Exercise also reduces stress and improves sleep.
However, extreme or intense exercise, especially without enough rest, can have the opposite effect. Very long or hard workouts can temporarily lower T cell counts and slow their response. This effect is often seen in endurance athletes who train heavily. Balance is key — regular, moderate exercise is best for immune support.
Diet and Nutrients
A healthy diet gives the body the vitamins and minerals it needs to produce and support T lymphocytes. Deficiencies in key nutrients can lead to lower T cell numbers and weaker immune responses.
Important nutrients for T cell health include:
- Protein: Needed for making all immune cells, including T cells
- Zinc: Helps T cells grow and function properly
- Vitamin C and Vitamin E: Support the defense system and protect T cells from damage
- Vitamin D: Helps regulate immune responses and supports T cell activity
- Iron and Selenium: Important for cell growth and immune signaling
Malnutrition, even mild, can weaken the immune system. A diet low in variety or too high in processed foods can lead to missing nutrients. Eating a wide range of fruits, vegetables, lean protein, whole grains, and healthy fats supports immune health.
Alcohol, Smoking, and Substance Use
Some lifestyle habits can harm T cells directly. Alcohol, when used in excess, damages the bone marrow, where immune cells are made. It also makes it harder for T cells to respond to infections.
Smoking introduces harmful chemicals into the body. These chemicals damage T cells and reduce their ability to move and function. Smoking also causes inflammation that may confuse or weaken the immune system over time.
Other substances, such as illegal drugs and even the misuse of prescription drugs like steroids, can also lower T cell levels or interfere with immune function.
Building a Resilient Immune System
Lifestyle choices do not act alone, but they do play a major role in shaping the immune system. Stress management, regular sleep, balanced exercise, good nutrition, and avoiding harmful substances help keep T cells healthy. Even when medical treatment is needed, these everyday habits support recovery and help the body stay ready to fight infections.
By understanding how daily life affects T lymphocytes, it becomes easier to make choices that strengthen immune health and reduce the chances of illness.
How Are Low T Lymphocytes Treated or Managed?
When the number of T lymphocytes in the body becomes too low, the immune system cannot work properly. This puts the body at higher risk for infections, delayed healing, and poor response to vaccines. The treatment for low T cell counts depends on what is causing the problem. In some cases, the immune system can recover on its own. In other cases, medical treatment is needed to help restore the body’s defenses.
Treating the Underlying Cause
The most important step in managing low T lymphocyte levels is to find and treat the cause. Low T cells may be due to infections, medications, cancer treatments, autoimmune diseases, or other health problems.
For example, if a viral infection such as HIV is the reason for the drop in T cells, then antiviral medications can help control the virus. When the virus is kept at a low level, the immune system has a better chance of rebuilding.
Some cancer patients lose T cells after chemotherapy or radiation. These treatments damage not only cancer cells but also healthy cells, including immune cells. After the treatment ends, the bone marrow often starts to produce more white blood cells again. Recovery may take weeks or months.
In autoimmune diseases like lupus, the body attacks its own immune cells. In these cases, doctors may use special medications that calm down the immune system without wiping it out completely. These medications can help protect T lymphocytes while controlling the disease.
If a medication is known to lower T cell counts, a doctor might change the drug or adjust the dose. Some drugs, such as corticosteroids or certain immunosuppressants, are known to lower lymphocyte numbers when used long term.
Protecting Against Infections
People with low T lymphocytes are more likely to get infections. Some of these infections can be serious or life-threatening. To reduce this risk, doctors may use antimicrobial medications as a preventive step.
For example, antibiotics or antifungal drugs may be given even if there is no current infection. This approach is called “prophylaxis.” It is often used in people with very low CD4 counts or those receiving organ transplants or chemotherapy. These medications help prevent common infections like Pneumocystis pneumonia (PCP), fungal infections, or certain viral reactivations.
Doctors may also recommend certain vaccines, but only non-live vaccines are safe when T cell levels are very low. Live vaccines, such as those for measles or chickenpox, may not be safe in individuals with weakened immune systems.
Immunomodulatory Therapies
Some people may benefit from medications that help the immune system recover or work better. These are called immunomodulatory therapies.
One example is interleukin-2 (IL-2), a natural protein in the body that can boost T cell growth. In some clinical trials, IL-2 has helped raise CD4 counts in people with HIV. However, it is not widely used because of possible side effects and mixed results.
Another option is thymic peptides, which are small proteins that help train T cells in the thymus gland. Some research has shown that they may support immune recovery, especially in older adults or after chemotherapy, though more studies are needed.
Hematopoietic growth factors, such as granulocyte colony-stimulating factor (G-CSF), can help boost white blood cell production in the bone marrow. While these do not directly raise T cell numbers, they may help improve overall immune function.
In rare and severe cases, such as genetic T cell deficiencies in children, bone marrow or stem cell transplantation may be considered. This can help rebuild the immune system with healthy donor cells, but it carries significant risks and is used only in very specific situations.
Multidisciplinary Care and Monitoring
Caring for a person with low T cell counts often requires a team of healthcare professionals. This may include infectious disease doctors, immunologists, oncologists, and primary care providers. Together, they monitor blood counts, check for signs of infection, and adjust treatment as needed.
Regular blood tests are important to track whether T cell levels are improving or getting worse. These include complete blood counts and tests that measure CD4 and CD8 cells. Doctors use these results to guide decisions about medications, vaccines, and lifestyle advice.
Supportive care is also part of the treatment plan. Good nutrition, adequate sleep, stress reduction, and avoiding exposure to infections all help protect the immune system. Some patients may benefit from counseling or support groups to manage the emotional stress of having a weakened immune system.
When Should You Be Concerned About Low T Cell Counts?
T cells are a very important part of the immune system. They help the body fight off viruses, bacteria, and other harmful things. When T cell levels drop too low, the immune system becomes weaker and less able to protect the body. While some people with low T cell counts may not feel sick right away, there are clear warning signs and risks that should not be ignored.
Common Warning Signs
One of the most common signs of low T cell counts is getting sick more often than usual. These infections might also be more serious or take longer to go away. For example, someone might get frequent colds, sinus infections, or skin infections that are harder to treat. There could also be more serious illnesses like pneumonia or blood infections.
Other warning signs include:
- Feeling tired all the time (fatigue)
- Losing weight without trying
- Having night sweats that soak clothes or sheets
- Swollen lymph nodes that do not go away
- Ongoing fevers or chills
These signs happen because the immune system is not working properly. When the body cannot fight off germs as it should, infections can keep coming back or last longer than normal. Even minor infections can turn into bigger problems. That is why these symptoms should be taken seriously.
Importance of Follow-Up and Monitoring
Doctors can check T cell levels with a blood test. The most common tests are a complete blood count (CBC) and flow cytometry, which measures the types and numbers of immune cells. It is also helpful to look at trends over time. One low result may not be a reason to worry, but a pattern of low counts can point to a bigger problem.
It is important not to ignore low T cell levels, even if there are no symptoms. A person might feel fine for a while, but the immune system may still be too weak to fight off infections later. Regular check-ups and repeat blood tests help doctors understand whether the immune system is recovering, staying the same, or getting worse.
Doctors may also do extra tests to find the cause of the problem. These tests could include looking for infections like HIV, checking for autoimmune diseases, or reviewing medications that might be lowering the T cell count.
People at Higher Risk
Some people have a higher chance of having low T cell levels. These groups need closer attention:
- People living with HIV/AIDS: HIV attacks and destroys CD4+ T cells. If the number of these cells gets too low, it becomes much harder to fight off infections. Regular monitoring is key for people with HIV to manage their immune health.
- Cancer patients and transplant recipients: Chemotherapy, radiation, and certain medicines used to prevent organ rejection can all lower T cell counts. These treatments are helpful for other health problems, but they make the immune system weaker. People in this group often need protection from infections and extra care.
- Older adults: The immune system naturally becomes weaker with age. The thymus, the organ that helps produce T cells, shrinks over time. This means fewer new T cells are made, and the ones that remain may not work as well. Older adults may not respond to vaccines as strongly, and they may recover from illness more slowly.
- People with autoimmune diseases: Some diseases like lupus or rheumatoid arthritis can affect how the immune system works. Medicines used to treat these conditions, such as steroids or biologics, can also lower T cell levels.
Prognosis and Long-Term Health
Low T cell levels do not always mean a person will become very sick. Some people improve once the cause is found and treated. For example, stopping a medicine that affects T cells or treating an infection can help counts return to normal. In other cases, low levels may last for a long time, especially in people with chronic illnesses.
Doctors may use low T cell counts as a clue to how serious an illness is or how likely a person is to recover. For instance, in people with cancer or HIV, very low T cell levels often mean the immune system is struggling. In these cases, doctors may take extra steps to help prevent infections or boost the immune system.
Paying attention to T cell levels can help avoid serious problems. With the right care and monitoring, it is possible to manage low counts and support immune health over time.
Can Low T Lymphocytes Recover or Normalize Over Time?
T lymphocytes, also called T cells, are an important part of the immune system. When the number of T cells is too low, the body becomes more vulnerable to infections and diseases. However, in many cases, low T cell counts can improve. Whether or not T cells return to normal levels depends on what caused the drop, the person’s overall health, and how the condition is treated.
Recovery After Temporary Suppression
Sometimes, T cell counts drop for a short period. This is called transient or temporary lymphocytopenia. It often happens during or after certain illnesses, especially viral infections like the flu, mononucleosis, or COVID-19. During an infection, the immune system works hard and uses up many of its cells. As the infection clears, the body begins to produce new T cells. In these cases, the number of T lymphocytes can return to normal in a few days or weeks.
Another common reason for temporary low T cells is treatment with certain medications. Chemotherapy, radiation, and immunosuppressive drugs can cause the immune system to slow down or stop making new T cells. After treatment ends, the body usually begins to recover. T cells often return to healthy levels, although this may take several weeks to several months depending on the treatment type and duration.
Factors That Influence Recovery
Recovery from low T cell counts depends on several factors:
- Age: Younger people usually have a stronger ability to rebuild T cells. The thymus gland, which helps produce new T cells, is more active in children and young adults. As people age, the thymus shrinks, making it harder to produce new T cells. Older adults may take longer to recover or may not fully return to normal T cell levels.
- Cause of the Low T Cell Count: If the cause is temporary or reversible, recovery is more likely. For example, recovery is more common after an infection or short-term medication. If the cause is long-lasting, such as a genetic immune disorder or HIV, T cell counts may stay low unless treated with specific therapies.
- Nutrition and Health: Proper nutrition plays a big role in immune recovery. Deficiencies in protein, vitamins, and minerals like zinc, iron, and vitamin D can slow down the production of T cells. A healthy diet with enough calories and nutrients helps the immune system recover faster. Other health conditions like diabetes, cancer, or chronic infections can also delay or prevent recovery.
- Medical Support: Some people need medical treatment to help boost T cell numbers. This might include antiviral drugs, antibiotics to prevent infections, or immune-boosting therapies. Regular check-ups help doctors track T cell levels and adjust treatment when needed. In some cases, bone marrow or stem cell transplants are used to rebuild the immune system, especially after cancer treatments.
Monitoring and Long-Term Planning
Doctors often monitor T cell counts through blood tests. A common test is the CD4 count, especially in people with HIV. When T cell counts are low, regular testing helps track recovery and guides treatment choices. If the count begins to rise steadily, it is a good sign that the immune system is getting stronger.
In some cases, the body may not fully return to normal T cell levels, but it may still function well enough to protect against most infections. The immune system has different types of cells that work together, so even with lower T cell numbers, people can remain healthy if other parts of the immune system are working properly.
Healthy lifestyle habits such as getting enough sleep, reducing stress, eating well, and avoiding smoking or alcohol can help the immune system recover. Physical activity also supports immune health by improving circulation and reducing inflammation.
Building Immune Resilience
Even if T cell numbers stay lower than normal, some people can live without serious problems if the rest of the immune system is strong. Doctors may recommend certain vaccines, medications, or lifestyle changes to support overall immune resilience. This means keeping the immune system as strong as possible to handle future challenges.
Over time, with proper care, the immune system often adapts. Many people with low T lymphocyte counts experience improvement, especially when the cause is treated early. Recovery is not always quick, but with attention to health and medical support, it is possible to rebuild a stronger immune defense.
Conclusion: Strengthening the Immune Frontline
T lymphocytes, also called T cells, are a key part of the immune system. These white blood cells help protect the body from infections, illnesses, and even cancer. When T cell levels drop too low, the body’s defense system becomes weaker. This makes it harder to fight off common viruses, bacteria, and other harmful organisms. It can also make infections last longer or become more serious. Low T cells can even allow old infections, which were once under control, to come back again.
T cells have many jobs. Some act like managers, telling other immune cells what to do. Others attack and kill infected cells directly. Each type of T cell has a special role, and together, they help keep the body healthy. Without enough T cells, the immune system cannot work the way it should. This condition, called lymphocytopenia, can be temporary or long-lasting, depending on the cause.
Many things can cause low T cells. Some are short-term, like viral infections or strong stress. Others are more serious, such as HIV, autoimmune diseases, cancer treatments, or inherited disorders. Sometimes, low T cell counts happen without a clear reason. In older adults, the number of T cells may slowly drop as part of aging. Poor nutrition, lack of sleep, or unhealthy habits like smoking and heavy drinking can also lower T cell levels.
Doctors can find out if T cell levels are low by using blood tests. These tests look at the number of lymphocytes and also break down the types of T cells, such as CD4 and CD8. Each type plays a different role. CD4 cells help direct the immune response, while CD8 cells destroy infected cells. A low number of either can be dangerous. Watching the balance between these two types, called the CD4/CD8 ratio, helps doctors understand how the immune system is working.
Having low T cells does not always mean something is wrong, but it can be a sign of a bigger health problem. When people start getting sick more often, or have infections that are hard to treat, doctors may check their T cell levels. In people with HIV or cancer, for example, keeping track of these levels is very important. Low T cells in these cases often mean a weaker immune system and higher risk of serious infections.
The good news is that in many cases, T cell levels can improve. If the cause is short-term, such as a cold or flu, the immune system often bounces back. Even after some medical treatments like chemotherapy, the body can rebuild its T cell supply over time. Eating a balanced diet, getting enough sleep, staying active, and reducing stress all support immune health. Avoiding alcohol and smoking also helps keep T cells strong.
In some situations, doctors use medicine to boost the immune system. These treatments are not for everyone and usually depend on the cause of the low T cells. Sometimes, people with very weak immune systems need extra care to avoid infections. They might need vaccines, antibiotics, or other medicines to stay safe.
T cells are like soldiers in the body’s defense system. When their numbers fall too low, the immune system becomes less able to protect the body. Learning about the causes of low T cells, recognizing the signs, and getting proper medical help can make a big difference. The immune system is complex, but it also has the ability to heal and grow stronger with the right support. Understanding T cells and taking care of the body helps the immune system stay ready for anything.
Questions and Answers
T lymphocytes (or T cells) are a type of white blood cell that play a central role in the immune response by identifying and destroying infected or cancerous cells and by regulating other immune cells.
Having low T lymphocytes, or lymphocytopenia, means that the body has fewer T cells than normal, which can impair the immune system’s ability to fight infections and diseases.
Causes include viral infections (like HIV), autoimmune diseases, malnutrition, certain cancers, chemotherapy, immunosuppressive drugs, and congenital immunodeficiencies.
Symptoms can include frequent or severe infections, fatigue, fever, weight loss, and slow wound healing.
It is diagnosed through blood tests, especially a complete blood count (CBC) and flow cytometry, which measure lymphocyte levels and subtypes.
A normal CD3+ T cell count ranges from about 1,000 to 1,800 cells per microliter of blood, though ranges can vary slightly by laboratory.
Yes, treatment depends on the cause and may include antiretrovirals for HIV, stopping immunosuppressive drugs, treating underlying infections, or immune-boosting therapies like IVIG.
HIV specifically targets and destroys CD4+ T lymphocytes, leading to immunodeficiency and increasing susceptibility to opportunistic infections.
CD4+ T cells help regulate immune responses, while CD8+ T cells (cytotoxic T cells) directly kill infected or cancerous cells.
Yes, people with low T cell counts may have a reduced response to vaccines because their immune system may not mount a strong or lasting defense.